Center for Clinical and Translational Science funds 18 new pilot studies
The Rockefeller University Center for Clinical and Translational Science (CCTS) has awarded 18 grants to university investigators in its third annual pilot-project grant program. The grants, which range from $2,000 to $25,000 each, will fund early studies in translational science that, if successful, might lead to improvements in human health. The CCTS, established through funds from a 2006 Clinical and Translational Science Award from the National Center for Research Resources of the National Institutes of Health, provided $365,000 for 17 projects over the first two years of the program.
The center’s Pilot Project review committee vetted proposals in the fall. The 2009 grant recipients are:
Donna Brassil, RN, CCRC, clinical research nurse facilitator, Hospital Program Direction, to compare the quality of blood samples obtained by two different methods of blood collection: intravenous catheters and venipuncture.
Manu Capoor, M.D., visiting scientist, Vincent A. Fischetti’s Laboratory of Bacterial Pathogenesis and Immunology, to devise a system to screen potential subjects for a clinical trial that will test the effectiveness of a particular lysin in reducing surgical site infections caused by Staphylococcus aureus.
Jules Cohen, M.D., instructor in clinical investigation, Ralph M. Steinman’s Laboratory of Cellular Physiology and Immunology, to assess the magnitude and quality of immune response to a novel vaccine against pancreatic cancer. Investigators will administer a monoclonal antibody, which targets dendritic cells, followed by a DNA plasmid that works as a booster.
Ype de Jong, M.D., Ph.D., visiting fellow, Charles M. Rice’s Laboratory of Virology and Infectious Disease, to define the feasibility of obtaining viable tumor cells from the blood of patients with metastatic liver cancer. Blood will be collected from patients and the samples used to identify tumor cells, which will then be cultured in vitro and/or injected into immunodeficient mice.
Emmanuelle Jouanguy, Ph.D., visiting assistant professor, Charles M. Rice’s Laboratory of Virology and Infectious Disease and Jean-Laurent Casanova’s Laboratory of Human Genetics of Infectious Diseases, to compare cytokine and gene expression profiles of immune cells from hepatitis C-positive patients with and without fibrosis, and to perform genome-wide association studies.
Michelle Lowes, M.D., Ph.D., assistant professor of clinical investigation, James G. Krueger’s Laboratory for Investigative Dermatology, to test the hypothesis that the primary skin symptom of neonatal-onset multisystem inflammatory disease — primary urticaria, or hives — is caused by increased production of interleukin-17, a cytokine involved in inducing and mediating inflammatory responses.
Jan Lunemann, M.D., postdoctoral fellow, to characterize the process by which major histocompatibility complex class II proteins — involved in presentation of antigens to T helper cells — work in mouse glial cells, and to identify substrates in central nervous system inflammation as candidate target antigens in this process. Results may eventually be applied in studies involving multiple sclerosis.
Patricia Maningat, M.D., instructor in clinical investigation, Jan L. Breslow’s Laboratory of Biochemical Genetics and Metabolism, to investigate the relationship between statin use and metabolic disorders.
Andreas Mauer, M.D., instructor in clinical investigation, Barry Coller’s Allen and Frances Adler Laboratory of Blood and Vascular Biology, to define the range of bleeding symptoms in healthy individuals using a newly developed, comprehensive electronic bleeding history immunophenotyping questionnaire.
Kristine Nograles, M.D., instructor in clinical investigation, James G. Krueger’s Laboratory for Investigative Dermatology, to evaluate the role of Th17 cells — helper T cells that protect the skin from extracellular bacteria — in juvenile psoriatic arthritis.
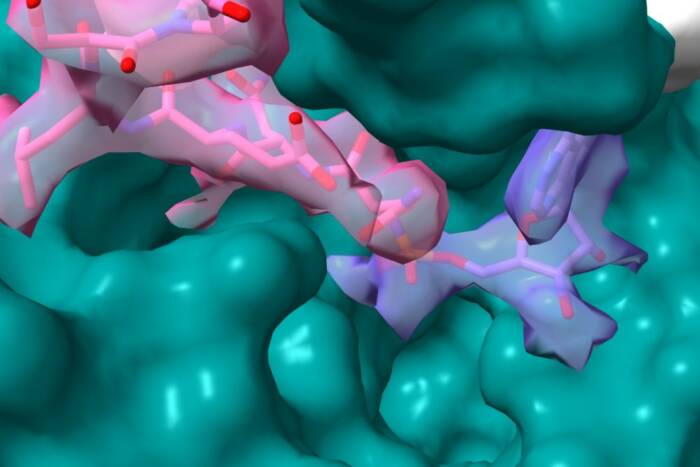
Mina Pastagia, M.D., instructor in clinical investigation, Vincent A. Fischetti’s Laboratory of Bacterial Pathogenesis and Immunology, to develop a temperature-stable and topically active formulation of ClyS, a newly developed lytic enzyme that is effective against multidrug-resistant strains and all other species of Staphylococcus aureus. This trial also aims to develop a skin mouse model to be used to ascertain the safety and efficacy of the formulation.
Alexander Ploss, Ph.D., postdoctoral associate, Charles M. Rice’s Laboratory of Virology and Infectious Disease, to generate mice that carry transplanted and functioning human genes, cells, tissues and/or organs for the study and intervention of human infectious disease.
Manish Ponda, M.D., instructor in clinical investigation, Jan L. Breslow’s Laboratory of Biochemical Genetics and Metabolism, to determine the effect of vitamin D3 repletion on endotoxemia and several biomarkers of atherosclerosis in patients with advanced chronic kidney disease and vitamin D deficiency.
Neil Renwick, M.D., Ph.D., instructor in clinical investigation, Thomas Tuschl’s Laboratory of RNA Molecular Biology, to identify proteins and mutations involved in Fragile X mental retardation and related disorders.
Johannes Scheid, visiting student, Michel C. Nussenzweig’s Laboratory of Molecular Immunology, to identify antibodies for a possible immune-based HIV vaccine, employing B cell lymphocyte sorting and immunoglobulin cloning techniques.
Jonathan Schmitz, biomedical fellow, Vincent A. Fischetti’s Laboratory of Bacterial Pathogenesis and Immunology, to mine the genomes of disease-causing bacteria for possible targets for the development of enzybiotics.
Christina Sobin, Ph.D., member of the adjunct faculty, Bruce S. McEwen’s Harold and Margaret Milliken Hatch Laboratory of Neuroendocrinology, to measure lead levels in a mouse model of chronic lead exposure.
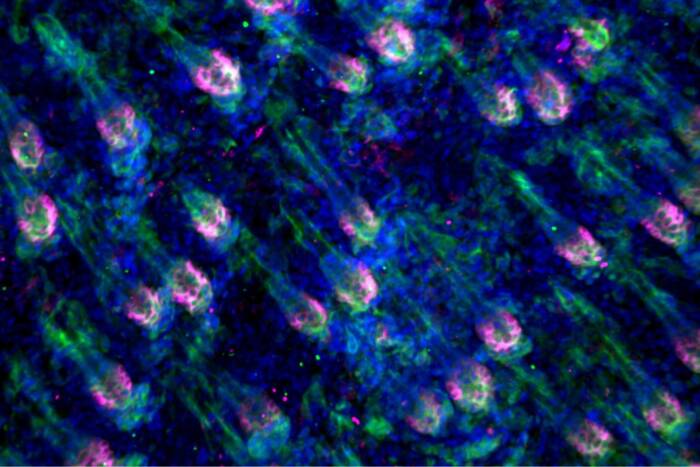
Lisa Zaba, Ph.D., biomedical fellow, James G. Krueger’s Laboratory for Investigative Dermatology, to define pathogenic dendritic cell subsets and maturation states present in human atherosclerosis, to compare the function of dendritic cells from atherosclerotic plaques compared to dendritic cells from psoriatic skin lesions and to perform gene expression analysis on cell subsets of atherosclerotic lesions.