Researchers uncover a pathway linked to autoimmune disease
When a person’s immune cells lose the ability to distinguish “self” from “non-self,” they end up launching an attack on the body they’re supposed to protect. Exactly what happens to rob them of that ability has been the subject of decades of research. In a series of discoveries that has the potential to help researchers halt autoimmune disorders — such as lupus and rheumatoid arthritis — one Rockefeller University scientist has found an underlying mechanism that begins to explain the pathologies of a number of immune diseases.
 (opens in new window)
(opens in new window)
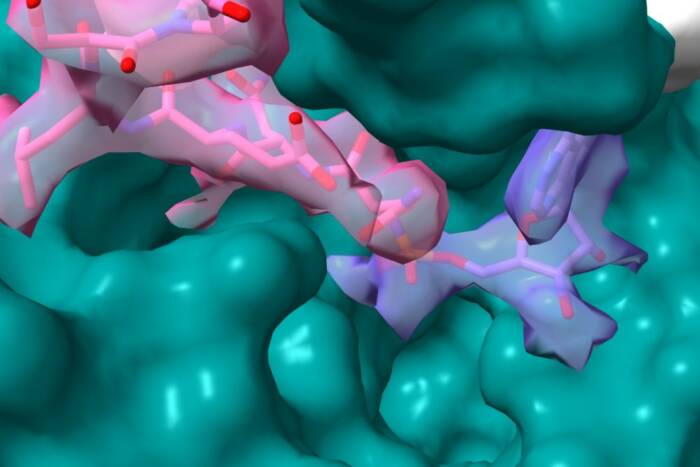
Immune dysfunction. An adaptor protein called MyD88 is a crucial element in the cellular pathway that, in the mouse model of lupus, causes immune cells to start reacting to DNA. When MyD88 is present, mice lacking a cellular receptor called FcγRIIB show an unusually high amount of the pathogenic IgG antibodies that cause inflammation in autoimmune diseases (green areas, left, from a mouse kidney). In mice that lack both FcγRIIB and MyD88, the accumulation of IgG2b antibodies is drastically decreased (right).
For years, Jeffrey Ravetch, the Theresa and Eugene M. Lang Professor and head of the Leonard Wagner Laboratory of Molecular Genetics and Immunology, has been working to untangle the complexities of how the body turns on itself. He’s accumulated evidence that immune cells go awry in a step-by-step process, and in two papers published in this month’s Journal of Experimental Medicine, he proceeds to nail down the last few steps by showing that the distribution of a class of proteins called immunoglobulins, or IgGs, can greatly affect the course of an autoimmune disease.
IgGs are a group of antibodies produced by plasma cells that bind to and activate specific immune cells, and they exist in various forms or “subclasses,” which bind to specific receptors (known as Fc receptors) on an immune cell’s surface; work by Falk Nimmerjahn, a postdoc in Ravetch’s lab, has demonstrated that the potency of these subclasses depends on which Fc receptors they engage. Now, Ravetch and his coauthors have shown that, in mice, a distorted ratio of these subclasses appears in at least two autoimmune diseases: systemic lupus and Goodpasture’s disease. Their finding blazes a new trail for researchers trying to treat these diseases, for it implies that they need to take aim at whichever IgG subclass has run amok. “For us, the lesson is that subclasses matter, because different diseases display skewing of various subclasses,” Ravetch says. “It’s important to know which subclasses dominate so you know which Fc receptors to target.”
In the lupus paper, co-written by visiting assistant professor Marc Ehlers, the scientists used a mouse model of the disease to determine how the immune system starts producing the wrong ratio of IgG subclasses. Previous work from Ravetch’s lab had shown that a specific Fc receptor is responsible for transforming immune cells into IgG-producing plasma cells — in lupus models, defects in this Fc receptor led to the build-up of IgG antibodies that attacked necessary cellular components such as DNA. But they didn’t know why the immune system began producing these so-called “anti DNA-antibodies” in the first place.
This study puts the last piece of the puzzle in place. Ehlers and Ravetch found that early on in their life, certain immune cells began to recognize and react to DNA — something they shouldn’t normally respond to. That DNA recognition then triggered a three-step process: A chemical pathway named “toll-like receptor 9” (which signaled with an adaptor protein called MyD88 and the transcription factor “T-bet”) led to antibody class-switching to the harmful IgG subclasses that ultimately lead to the disease. “This begins to explain the progression of a disease like lupus,” Ravetch says. “And if you block any step in the pathway, you don’t get the disease.”
The second paper, which Ravetch co-wrote with postdoc Yoshikatsu Kaneko, addresses the mouse model of Goodpasture’s disease, a rare disorder in which autoantibodies attack the lungs and kidneys. Ravetch and Kaneko show that this kidney disease, like lupus, also shows unnaturally high levels of one particular IgG subclass, IgG2b. That subclass binds to a specific Fc receptor on immune cells that activates them, leading to an upsurge in inflammation. And once the researchers had that information, they were then able to intervene and reverse the course of the disease. By giving the mice intravenous immunoglobulin (IVIG) — a solution of IgG antibodies found in healthy blood — they could change the ratio of Fc receptors on immune cells, thereby increasing the number of IgG2b antibodies necessary to trigger inflammation, and effectively stopping the disease in its tracks.
“These new findings highlight the importance of IgG subclasses in autoimmune diseases,” Ravetch says. “And they provide several new targets for preventing their generation, accumulation or pathogenicity.”
Journal of Experimental Medicine 203(3): 789-797 (March 20, 2006)(opens in new window)