PLD1 protein is implicated in Alzheimer's brain damage
Most current Alzheimer’s drugs target molecules responsible for memory formation. But while helpful at slowing and even reversing memory loss, this approach doesn’t address the root of the problem: plaques that build amid brain cells, causing them to weaken and die.
 (opens in new window)
(opens in new window)
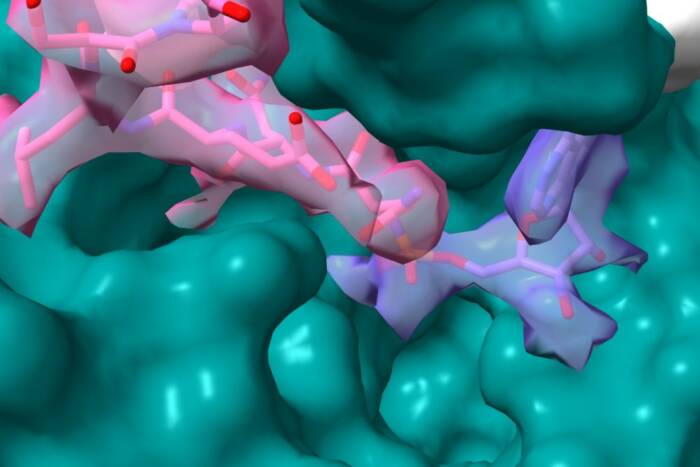
Plaque fighter. Rockefeller University scientists say that a protein called PLD1 may be a target for new drugs that better treat Alzheimer’s disease. Among their findings: impairment of neurite outgrowth (left) in mouse brain cells that mimic the early-onset disease found in humans was reversed by adding PLD1 (right).
In back-to-back papers published online in Proceedings of the National Academy of Sciences, Dongming Cai and other Rockefeller scientists, in the research group led by Paul Greengard, now say that a protein called PLD1 may be a target for new drugs that better treat — or even prevent — Alzheimer’s. PLD1, the scientists say, plays two major roles in the cellular processes that lead to damaged brain cells in Alzheimer’s disease. First, PLD1 regulates the shuttling of beta-amyloid precursor protein (beta-APP), a large molecule produced naturally in the body and found in many different cells, including brain cells. Second, PLD1 inhibits formation of beta-amyloid, the protein fragment responsible for the brain plaques found in Alzheimer’s patients, by altering the function of an enzyme called gamma-secretase.
“These combined actions of PLD1 raise the possibility that therapeutic approaches targeting this enzyme could be developed for restoring neuronal dysfunctions in Alzheimer’s disease,” says Greengard, who is Vincent Astor Professor and head of the Laboratory of Molecular and Cellular Neuroscience at Rockefeller and also director of the university’s Fisher Center for Research on Alzheimer’s Disease.
Beta-APP travels through a part of the cell known as the trans-Golgi network on its way to the cell surface. Most scientists believe that the longer the protein stays in the trans-Golgi network, the more likely it is to develop into beta-amyloid. Scientists say that beta-amyloid is formed when gamma-secretase, and its sister enzyme beta-secretase, chop up beta-APP. The researchers focused on how a protein called presenilin-1, which regulates the cleavage of beta-APP and its trafficking within the cell and is a culprit in some early-onset forms of Alzheimer’s, interacts with PLD1.
To better understand the pathways involved, Greengard and his team experimented with adding PLD1 to brain cells from mice that mimic the early-onset disease found in humans. Under normal conditions, these cells show an impairment of neurite outgrowth, the process by which neurons become assembled into functional networks. But adding PLD1 to these cells improved neurite outgrowth by regulating the intracellular trafficking of beta-APP.
The researchers also found that the effect of PLD1 on trafficking occurs through a mechanism independent of its effect on the gamma-secretase complex. Thus, when they increased levels of PLD1 in cultured cells harboring familial Alzheimer’s disease (FAD)-linked presenilin mutation, they observed a decrease in the amount of beta-amyloid produced.
“The discovery that one can affect the rate of beta-APP metabolism by changing PLD1 levels suggests a novel therapeutic approach for delaying or preventing Alzheimer’s disease,” says Greengard.
The project was a collaboration with scientists at Hunter College of the City University of New York, Baylor College of Medicine, Albert Einstein College of Medicine, University of Chicago, Yale University and the Burnham Institute for Medical Research.
Proceedings of the National Academy of Sciences 103(6): 1936-1940 (February 7, 2006)(opens in new window)
Proceedings of the National Academy of Sciences 103(6): 1941-1946 (February 7, 2006)(opens in new window)