Unique characteristics of a rare liver cancer identified as clinical trial of new treatment begins

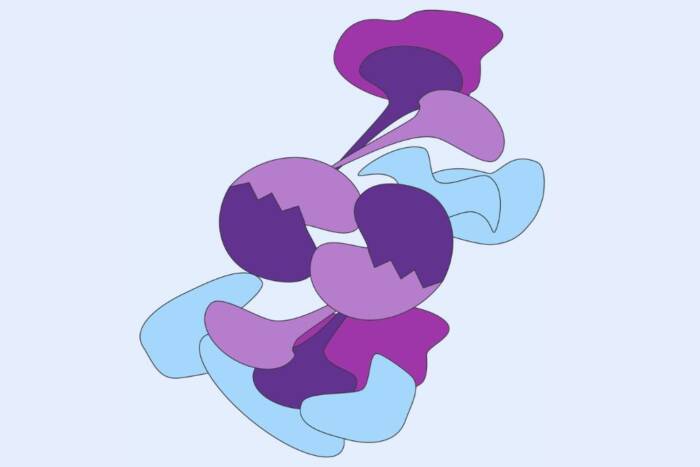
Histological section of an FLC tumor, showing the stromal (left), normal (center), and tumor (right) cells. The colors correspond to gene markers identified for different cell types. (Simon Lab)
Like many rare diseases, fibrolamellar hepatocellular carcinoma (FLC) mounts a ferocious attack against an unlucky few—in this case, children, adolescents, and young adults. Because its symptoms can vary from person to person, it’s often missed or misdiagnosed until it has metastasized and becomes lethal. Moreover, drug therapies for common liver cancers are not just useless for FLC patients but actually harmful.
But new insights about the disease, coupled with a just-launched clinical trial of a promising drug treatment, could significantly improve health outcomes. Researchers in Rockefeller University’s Laboratory of Cellular Biophysics, headed by Sanford M. Simon, has discovered that FLC has a distinct transcriptomic “signature”—a set of activated genes—that makes it unique among liver cancers.
“Identifying which molecular changes characterize FLC is an important step to understanding how it arises and evolves, which may reveal potential therapeutical targets,” says first author David Requena, a senior researcher in the lab. “Ideally, our findings will refine the detection of the disease, change the course of treatment, and increase patient survival rates.”
The findings, published(opens in new window) in Nature Communications, come as Simon’s lab begins a clinical trial that pairs two drugs into one treatment that preliminary results indicate is highly effective against FLC.
A decade of insights
In 2014, Simon’s team—led in part by his own then-teenage daughter, Elana, who had been diagnosed with FLC a few years before—discovered(opens in new window) that the disease was caused by the fusion of two genes, DNAJB1 and PRKACA, caused by a small deletion in chromosome 19.
The lab recently determined that what is important is not formation of the fusion, but that the formation results in an increase of the amount of PRKACA—the catalytic subunit of protein kinase A—that is made. That is the true origin of the disease. FLC tumor cells essentially have a molecular imbalance: too many catalytic PKA proteins and not enough of the inhibitory ones that normally tamp down the protein and lock it into place. Unfettered, overabundant PKA is free to wreak havoc across the cell.
For the current study, the researchers wanted to know if there is a common pathway of disease following the burst of PKA proteins. Some liver tumors are categorized as “FLC-like” but lack the fusion protein. Are they actually FLC? And since FLC is impervious to treatments that inhibit other liver cancers, what differentiates it from these other malignancies?
The signature
To find out, the researchers performed a massive analysis of multiomics sequencing data from 1,412 tumors caused by a variety of liver cancers. It was the largest such analysis to date, with 220 samples from FLC tumors—more than six times as many as have been included in any prior study.
In this way, the team determined the transcriptomic signature of each tumor, revealing which dysregulations are unique to specific tumor types and which are common to all. Single-cell analysis with spatial resolution further helped them to identify how each cell type in the tumor contributes to the overall transcriptome.
The result: FLC emerged as a distinct outlier. “We identified 301 genes that were expressed differently in FLC than they were in other tumors, which really underscores how unique it is among liver cancers,” Requena says. “Moreover, 35 of those were highly expressed only in FLC. These genes could be tested for diagnostic applications in the clinic.”
They also found that any change in DNA that increased the amount of catalytic subunit relative to its regulatory subunit produced the same changes in the transcriptome. Some patients, for example, had a fusion to PRKACA in the ductal cells of the liver, producing cholangiocarcinoma, or in the ductal cells of the pancreas, producing intraductal pancreatic oncolytic neoplasms (IOPNs). Even though these were different fusions to PRKACA and were identified in cells other than hepatocytes, where FLC is found, they produced the same changes in the transcriptome. And some patients were only missing the regulatory subunit but still had the same changes.
Recently, the Simon Lab also demonstrated(opens in new window) that these diseases responded to therapeutics in the same way that FLC does.
“Thus, we suggest that the cancer perhaps should be defined not by its DNA change but by the change it produces in the net balance of protein activity in the cell,” says Simon, the Günter Blobel Professor at Rockefeller.
They also compared the tumor transcriptomes against those of normal tissue samples taken from the margins of tumors found in FLC patients. Surprisingly, one had the FLC signature. Upon closer re-examination of the tissue, they spotted fibrous spans typical of the disease and cells that had the fusion transcript of DNAJB1::PRKACA. Removal of the tumor hadn’t captured all FLC cells. Such hidden time bombs could result in new cancer growth.
“This finding really demonstrates the importance of a complete examination of the margins of the tumor,” says Simon.
A promising clinical trial
With these insights in hand, the researchers have just begun a clinical trial(opens in new window) to test the pairing of two anti-cancer medications, DT2216 and irinotecan, that the lab’s earlier research, published in 2022(opens in new window), indicated are effective against FLC when used in combination. This is being supported by the Children’s Oncology Group and the Pediatric Early Phase Clinical Trials Network of the NIH.
In parallel, the Simon Lab is also developing alternative therapeutics, an effort supported by the Cancer Grand Challenge, a highly competitive initiative by Cancer Research (UK) and the National Cancer Institute (US) that offers $25 million grants over five years to consortiums of researchers working towards similar goals. Simon’s lab is part of the KOODAC team, in which different labs are attempting to degrade an oncoprotein—in Simon’s case, fusions with PRKACA—to prevent or kill tumors. Simon aims to present their findings at the annual meeting of the American Association for Cancer Research in late April.
“Ten years ago, it was our hope that by focusing on comprehensively characterizing a single, albeit rare, disease we could made rapid progress on developing both diagnostics and therapeutics that would not only advance FLC treatment but provide a roadmap for other diseases,” he says. “The recent findings from our group validate that hope and offer the promise that these insights can be translated not just to other cancers—such as Ewing sarcoma, rhabdomyosarcoma, and neuroblastoma—but also to illnesses in which we have to eliminate a protein that is not functioning properly.”