Leukemia drug Gleevec slows accumulation of major component of senile plaques in cell studies and in guinea pigs
Gleevec, the breakthrough drug for treating chronic myologenous leukemia (CML) and gastrointestinal stromal tumors, slowed the accumulation of the major protein component of senile plaques that characterize Alzheimer’s disease, in laboratory cultures of mouse brain cells and guinea pigs.
The findings, reported by a team of researchers at The Rockefeller University’s Fisher Center for Alzheimer’s Disease Research and Memorial Sloan-Kettering Cancer Center (MSKCC) in the Sept. 29 online edition of Proceedings of the National Academy of Sciences, show that Gleevec and a related chemical compound reduced the buildup of a small molecule called beta-amyloid peptide, which makes up the senile plaques found in the brains of most people with Alzheimer’s.
Importantly, neither Gleevec nor the other compound inhibited another protein that is crucial for the normal functioning of the immune system. Previous research by other scientists on other beta-amyloid inhibiting compounds demonstrated that most of these agents also inhibited the crucial immune system protein, which is called Notch.
“The safety of Gleevec, which has already been shown through its use in treating CML and gastrointestinal stromal tumors, combined with its inability to inhibit Notch, make this class of compounds an attractive lead for the development of a potentially safe treatment for Alzheimer’s,” says principal investigator Paul Greengard, Ph.D. Greengard, who is a Vincent Astor Professor and director of the Fisher Center for Alzheimer’s Disease Research at The Rockefeller University, received the 2000 Nobel Prize in Physiology or Medicine.
“Alzheimer’s disease is an insidious mental disorder that affects an estimated four-and-a-half million Americans,” says Paul Nurse, Ph.D., Rockefeller University’s new president and recipient of the 2001 Nobel Prize in Physiology or Medicine. “Paul Greengard and his colleagues have discovered a very exciting application of an already well-tested drug. However, we must keep in mind that these experiments now need to be repeated in human patients.”
Greengard also noted that while Gleevec shows promise in cultured laboratory cells and guinea pigs, it is not suitable in its present form for treating people with Alzheimer’s: the molecule that makes up Gleevec does not cross the blood-brain barrier, the gatekeeper that prevents some substances in the blood from entering the brain. For this study, Gleevec was administered to the guinea pigs through the cerebrospinal fluid.
“It’s possible that Gleevec could be chemically modified to cross the blood-brain barrier,” says first author William Netzer, Ph.D., a research associate in Greengard’s lab. “Or there may be other compounds that function like Gleevec but are chemically suited to enter the brain. It’s a very promising area.”
In studies of laboratory cultures of mouse neuroblastoma cells in 1999, Greengard’s team showed that beta-amyloid production depended on a chemical reaction involving ATP, a small molecule that plays a critical role in the storage and release of energy within cells in the body. The Rockefeller University researchers hypothesized that inhibiting ATP could be an avenue to reducing the production of beta-amyloid in people with Alzheimer’s disease.
Most researchers believe these plaques or the beta-amyloid fragments are the cause of Alzheimer’s, whose devastating effects include memory loss, dementia and ultimately death.
In a naturally occurring process, beta-amyloids form when protein-cutting enzymes, called beta- and gamma-secretase, chop up the amyloid precursor protein, a large molecule produced naturally in the body and found in many different cells. In Alzheimer’s disease, excess beta-amyloids cause nerve cells in the brain to weaken and die.
The Rockefeller researchers took a close look at Gleevec because of its success in treating CML, which is caused by a mutant enzyme called BCR-Abl. Gleevec selectively blocks BCR-Abl, as well as the normal enzyme, called Abl, without harming many of Abl’s molecular cousins. In 2001, researchers at Rockefeller, the Howard Hughes Medical Institute at the university and MSKCC showed that Gleevec blocks Abl by partially mimicking ATP and binding tightly to an area on Abl that is normally occupied by ATP.
Abl belongs to a larger family of proteins called tyrosine kinases, which act like biological switches and play important roles in regulating cell growth and division. Gleevec has been shown to bind to a handful of other tyrosine kinases.
“There are over 1,000 proteins in human cells that use ATP to function, and possibly 800 of these are kinases,” says Netzer. “We know that Gleevec binds to at least four tyrosine kinases, most of which are distantly related to one another in evolutionary terms, so we took a gamble that the set of ATP-utilizing proteins targeted by Gleevec could be much larger.”
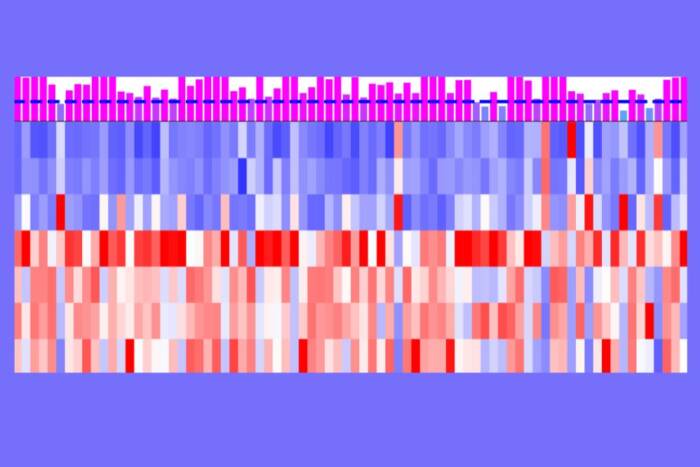
Using laboratory cultures of mouse neuroblastoma cells that make human APP, the Rockefeller researchers found that beta-amyloid production decreased with the addition of Gleevec and that this was due to an inhibition of gamma-secretase. The researchers also tested Gleevec on brain cells taken from rats that contained no human APP and obtained similar results. This showed that Gleevec’s effect on beta-amyloid production was not restricted to cell lines containing human beta-amyloid.
To test the effects of Gleevec in living animals, the researchers injected Gleevec directly into the spinal fluid of guinea pigs. They chose guinea pigs because guinea pigs and humans have chemically identical beta-amyloid. This similarity allowed them to use a technique called “sandwich ELIZA” to analyze the results.
The Rockefeller researchers found that Gleevec reduced levels of beta-amyloid in the guinea pigs. They also tested a non-clinical compound provided by the Synthetic Organic Chemistry Core Facility at MSKCC. Referred to as “inhibitor 2,” in the PNAS paper, this compound blocks a cancer-promoting tyrosine kinase called Src (pronounced “sark”) as well as most of the tyrosine kinases that are known to be inhibited by Gleevec.
The Rockefeller research group believes that Gleevec and a related inhibitor used in the study reduce the production of beta-amyloids by impairing the function of gamma-secretase. It’s still not clear, however, if Gleevec acts directly on gamma-secretase or another molecule that regulates it. However, the researchers have shown that Abl is not responsible for the effect of Gleevec on beta-amyloid production.
In the last few years, other scientists searching for ways to reduce beta-amyloid production have identified other inhibitors of gamma-secretase. However, most of these inhibitors also block the cleavage of the important immune system molecule called Notch. Notch belongs to a family of proteins called transcription factors, an essential group of proteins responsible for turning genes on and off. Specifically, Notch plays a pivotal role in the development of blood-forming organs and the immune system.
In order for Notch to perform its jobs properly, it needs to be cut, or cleaved. Malfunctions in Notch cleavage can lead to a particular form of T-cell leukemia.
Netzer’s and Greengard’s co-authors are Fei Dou, Dongming Cai, Stephanie Jean, and Huaxi Xu, at Rockefeller and Darren Veach, Yueming Li, William G. Bornmann, and Bayard Clarkson at MSKCC.
This research was supported by the National Institutes of Health and by generous support from the Fisher Foundation for Alzheimer’s Disease Research.