Many Immune Cells Are Fine-tuned to Prevent "Friendly Fire"
Body salvages cells by altering genes during halt in development

Rafael Casellas
About one-quarter of the body’s antibodies are produced by immune cells that have had their genetic code revised during a halt in their development, scientists at Rockefeller University and three other institutions have found. The study is the first to show that this phenomenon, called “receptor editing,” plays a major role in the creation of the body’s huge antibody array.
Receptor editing allows the body to modify potentially harmful immune cells rather than destroy them, a maneuver that conserves energy while maintaining an immune system that is both strong and safe. The research, published in the Feb. 23 issue of the journal Science, sheds light on a crucial stage in which the body shapes its immune defenses.
“This is the first experiment designed to measure how often receptor editing occurs in a live animal,” says lead author Rafael Casellas, a graduate student who works in the Laboratory of Molecular Immunology at Rockefeller. “Until now, all we knew is that editing can happen. This study proves that it is happening to a surprising extent.”
The prevailing view of how the immune system achieves “tolerance” has been that troublesome immune cells are never allowed to develop to the point where they can produce antibodies–the body simply eliminates or enfeebles the entire cell. The idea that so many cells are instead fine-tuned and allowed to progress will cause immunologists to revise the model by which they understand the system.
“It is quite striking that what is being targeted so often is not the B cell per se, but a specific part of the antibody–the receptor–that the cell produces,” Casellas says. “It is a much finer distinction, one that the body makes more than most of us suspected.”
B cells in humans and other vertebrates create antibodies with surface receptors that fit specific antigens. When a foreign substance invades the body, it is the antigen that selects the B cell with the proper antibody, which causes the cell to multiply to launch an immune response. (Although there are many B cells, each one produces only one specific antibody.)
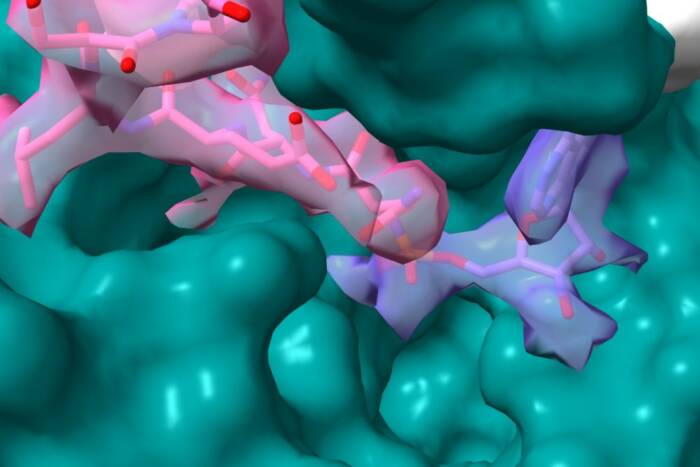
The body manages to create a huge number of unique antibody molecules with a relatively small number of genes by recombining several gene segments into a patchwork gene that encodes a Y-shaped antibody with a highly specific receptor on its arms. The antibodies are randomly made to fit any conceivable antigen they might encounter. This random production inevitably creates antibodies that will attack the body’s own proteins, meaning that a significant number of immune cells are potentially harmful.
To address this threat, the body employs various mechanisms to prevent this from happening, of which four have been discovered so far. Three of the four involve targeting the B cell before it develops enough to produce the harmful antibody. In some cases, the body simply destroys the B cell–a process called “central deletion.” This method was first proposed by Rockefeller University Nobel Prize-winner Joshua Lederberg in 1959 but not proven until about 10 years ago.
More recent research has uncovered three other strategies. Some cells undergo a process called “anergy,” in which the cells are disabled and die a slow death. In rare cases, called “ignorance,” the cells simply fail to respond to the antigen for which they were designed. The fourth mechanism, receptor editing, is the only one that alters the antibody and allows the cell to move on.
The modification to the cell in receptor editing is not extensive. But since antibodies are so highly specialized, a minor change can still have a big impact–much the way a slight imperfection on a key can render it useless.
Although changing the cells in such a manner benefits the body, the editing itself is haphazard in that the alteration is not guided so that a specific sequence is inserted when the new gene is patched together. Rather, the body splices in a random sequence and sees if it works. If the cell is still self-reactive with its new receptor, it once again is subject to one of the body’s four protective mechanisms.
Casellas and his colleagues conducted their experiment with genetically modified mice that allowed them to determine whether a specific DNA stretch had been changed during immune system development. They inserted a human DNA sequence into a precise spot in the mouse genome and waited to see how often it showed up in the B cells after the animals had developed.
They found that 25 percent of the light chains on the surface of developing B cells were produced by receptor editing. Further, that editing occurs in the B cells during a two-hour delay in development, at a stage in which they are normally recombining their light chain genes.
“The body senses that the B cell is self-reactive, so it halts the cell to be modified during that early stage in development,” Casellas says.
This type of finding became possible only through the development of innovative genetic manipulations that allow researchers to target precise DNA locations to ask specific questions.

Michel C. Nussenzweig
“The technology is allowing us to develop sophisticated systems aimed at answering very specific questions about immunity and tolerance,” says corresponding author Michel Nussenzweig M.D., Ph.D., Rockefeller professor and investigator with the Howard Hughes Medical Institute. “Use of these ‘knock-in’ genes should lead us to a much clearer understanding of how the body codes for its antibodies.
The study was funded in part by the National Science Foundation, the National Institutes of Health and Deutsche Forschungsgemeinschaft.