Researchers find how leprosy bacterium selects and attacks nerves

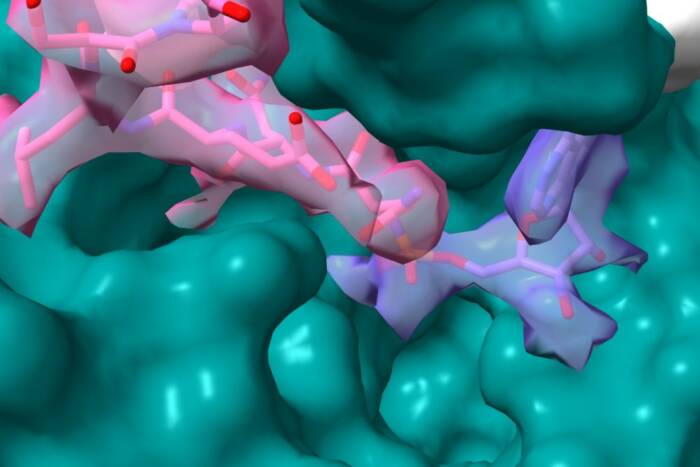
A schematic drawing showing in vivo interaction of the leprosy bacterium M. leprae with the basal lamina of a myelinated Schwann cell-axon unit.
Mode of invasion may provide clues to the early events of other neurological diseases
Researchers at Rockefeller University who study the bacterium that causes leprosy say they have identified a component on the microbe’s surface that allows it to specifically select and attack the peripheral nerves. The finding clarifies how the bacterium, Mycobacterium leprae (M. leprae) precisely seeks out peripheral nerves, and it sheds light on the early stages of nerve damage in other neurodegenerative diseases such as Guillain-Barre syndrome and multiple sclerosis.
“If we can understand what neural cell molecules the bacteria use to infect the nerves, we’ll gain more insight into what kinds of signaling pathways are involved in bacterial-induced nerve degeneration,” says Anura Rambukkana, Ph.D., principal investigator and research associate in the Laboratory of Bacterial Pathogenesis.
In addition, learning what M. leprae does to perturb neural signaling may help researchers understand how the pathway normally works–a process that is still poorly understood. The research was reported in the Oct. 27 issue of the journal Cellby Rambukkana together with Vincent Ng, a graduate student at Rockefeller, and researchers at three other institutions.
The peripheral nervous system consists of all the nerves that fan out from the brain and spinal cord and includes the muscles, skin and internal organs. During development, Schwann cells encase nerve fibers and wrap around the axon to form the myelin sheath. This sheath greatly improves the reliability and speed of the electric impulse, much like insulation on electrical wires. When myelin is damaged, as withM. leprae infection and in patients with Guillain-Barre syndrome and multiple sclerosis, the nerve fibers are no longer insulated and nerve impulses cannot be conducted efficiently. The Schwann cell-axon unit is surrounded by an outer layer called the basal lamina, a matrix secreted by the Schwann cells. The components of the basal lamina that are targeted by M. leprae play a vital role in myelination.
Rambukkana and colleagues previously reported that a major component in the Schwann cell basal lamina, called lamina-2, and its receptor, called dystroglycan, are involved in M. leprae’s interaction with Schwann cells. This interplay allows the bacterium to infect the peripheral nerves, which eventually causes nerve damage.
The new research focuses on the invader’s side of the interaction–specifically, on identifying the part of the microbe’s cell wall that allows the interaction to occur.
The cell wall of M. leprae is endowed with large quantities of a glycolipid called phenolic glycolipid (PGL-1). PGL-1 contains a trisaccharide unit that exists only in M. leprae. This uniqueness led researchers to speculate that PGL-1 plays an essential role in functions that are specific to the leprosy bacterium–such as infecting peripheral nerve cells–but they had no proof.

A micrograph illustrating that same interaction being reproduced in vitro in nerve tissue culture; M. leprae is binding to a mylenated nerve fiber (the oblong Schwann cell nucleus shown in blue is an indicative of the myelinated nerve fiber)
Now the researchers have demonstrated that PGL-1 binds specifically to native laminin-2 but not to other proteins in the basal lamina of the Schwann cell-axon unit. It turns out that invasion of the Schwann cell is ultimately controlled by the neural target, not the invading microbe. The basal lamina is a dynamic action zone that functions to instruct neural cell phenotypes and activation. Modulation of the basal lamina has profound effects both on its function and the consequent behavior of cells residing within it. Therefore, it is not surprising that the basal lamina and Schwann cells respond to PGL-1 upon contact with the bacterium by opening the pathway to allow the intruder to enter.

A schematic showing the chemical structure of PGL-1, a unique M. leprae surface component that mediates the interaction by binding to the G domain of laminin-2 in the Schwann cell basal lamina.
“We think clarifying PGL-1’s role in nerve infection will eventually make it possible to develop strategies to block bacterial invasion of the peripheral nerve cells at an early stage and thus prevent neurological damage before the immune system gets involved,” Rambukkana says.
Leprosy is a chronic bacterial infection that damages nerves, mainly in the limbs and facial area, and also leads to skin lesions. M. leprae is the only known human bacterial pathogen that attacks the Schwann cell of the peripheral nervous system, and the nerve damage it induces is by far one of the leading cause of peripheral nerve disease in the world. The disease can be treated with multidrug therapy that kills most of the M. leprae in a few weeks. However, nerve function loss caused by M. leprae invasion of Schwann cells is irreversible.
Rambukkana and his colleagues are now focusing on how neurotropic pathogens, both M. leprae and viruses, attack the peripheral nervous system, and they hope to use these pathogens and their products as tools to identify early molecular events of neurodegenerative diseases. The researchers will focus especially on demyelinating diseases, both those of infectious origin–known to be caused either by bacteria or viruses–and those with unknown causes, such as Guillain-Barre syndrome and multiple sclerosis.
The other co-authors of the Cell paper are George Zanazzi, B.S., and James Salzer, M.D., Ph.D., of New York University Medical Center; Rupert Timpl, Ph.D., and Jan F. Talts, Ph.D., of the Max-Plank-Institüt for Biochemistry in Germany; and Patrick Brennan, Ph.D., of Colorado State University.
The research was supported by grants from the National Institutes of Health and the UNDP/World Bank/WHO Special Program for Research in Tropical Diseases.