Rockefeller University Researchers Find Large Hole-Forming Protein in Bacteria -- A Potential Achilles' Heel?
Finding Opens Door on Dysentery, Bubonic Plague, Cholera and Salmonella Poisoning
Researchers at The Rockefeller University have shown for the first time that a protein called pIV forms a hole in the outer membrane of the bacterium E. coli to allow passage of large molecules. The finding, reported in the May 28 issue of the journal Science, may allow researchers to exploit the bacterium’s Achilles’ heel to better deliver antibiotics.
A clearer understanding of how bacteria use this channel to import and export large molecules could one day lead to new strategies for fighting pathogens such as Shigella, Yersinia, Vibrio cholerae, and Salmonella, the causative agents of dysentery, bubonic plague, cholera and gastroenteritis respectively.
The pIV protein is made by filamentous phages—viruses that infect bacteria—and is required for newly assembled phage particles to exit the host bacterial cell. The researchers have shown that pIV forms a large channel that is normally closed.
“Knowing that the bacteria must normally keep this channel closed when not in use allowed us to look for and find variants of the channel which would open inappropriately,” says co-author Marjorie Russel, Ph.D. “This provided an important clue to observing this channel.”
“The observation that many different bacteria have a protein that is very similar to pIV has generated a lot of interest in how phages are exported. These bacterial proteins are known to be involved in exporting toxins required for bacterial virulence,” according to co-author Denise Marciano, A.B.
“Proving that this channel exists and demonstrating how it works is very important to understanding the many pathogens that have plagued humanity, literally and figuratively,” says study co-author Sanford Simon, Ph.D. “The membranes that surround a cell are effectively a sea wall that is essential for survival. However, just to push the metaphor, no cell is an island. In order for a cell to survive, its membranes must take up nutrients from its surroundings and get rid of waste materials while still keeping other substances from crossing the barrier. Many pathogens have the further challenge of trying to maintain this sea wall to protect themselves while they are trying to export large toxins to attack our cells.”
Researchers already knew that cells take in selected items like potassium or sodium ions through very small, water-filled pores, and within the last 10 years, Simon and Rockefeller colleague Günter Blobel, M.D., Ph.D., an investigator at the Howard Hughes Medical Institute, identified larger, water-filled channels with gates that open to let proteins cross the membrane. But this did not explain how even larger molecules, including phages and large toxins, managed to cross these membranes without compromising the health of the cell.
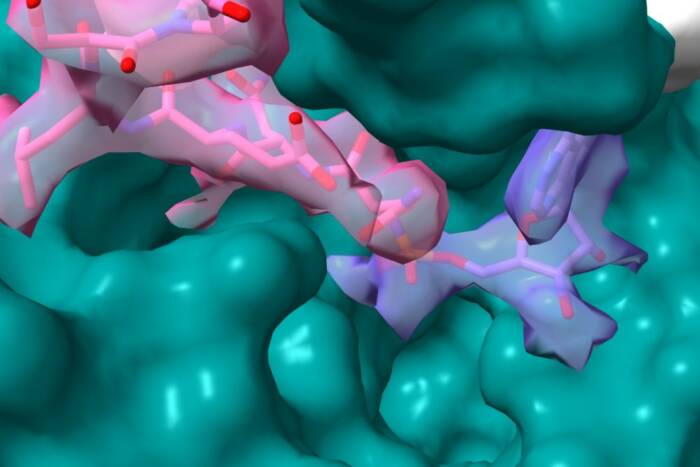
To answer this question, Marciano, Russel and Simon studied how filamentous phages get out of E. coli. The phages reproduce inside E. coli cells and are continuously exported from the cells, without killing or bursting the bacteria. In previous research, Russel found that pIV forms a cylinder-shaped complex inE. coli’s outer membrane that is just wide enough to allow export of the elongated phage.
The latest research confirms pIV’s role as a portal and shows that the channel opens and closes in response to a change in the voltage of the membrane. It is the largest channel yet recorded that operates through this type of electrical signal. The identification of these mechanisms suggests that it may be possible to trick the channels to open inappropriately so that specially designed drugs could enter bacterial cells and destroy them.
“This work is a fine example of the strengths of an institution like Rockefeller that has no departmental walls,” Simon says. “It allows interdisciplinary work-in this case a geneticist and a biophysicist addressing an important issue in microbiology and cell biology.”
This research was supported in part by a grant from the National Institutes of Health’s Medical Science Training Program, by the National Science Foundation and by the Keck Foundation.