Bacteria Steal Genes, Spread Antibiotic Resistance
Multidrug-Resistant Streptococcus Switches Coat to Evade Immune System
A strain of the bacterium Streptococcus pneumoniae, resistant to the six most frequently used antibiotics and spread worldwide including U.S. day care centers and hospitals, appears to disguise itself from the immune system by changing its coat, report scientists from The Rockefeller University.
“We found a strain of multidrug-resistant Streptococcus pneumoniae that appears to have taken genes from another strain to switch its coat and evade the immune system,” says Alexander Tomasz, Ph.D., head of the Laboratory of Microbiology at Rockefeller. “This method of disguise could be a major contributor to the worldwide spread of resistance to antibiotics like penicillin. What we have learned may be useful for designing new anti-pneumococcal vaccines.”
S. pneumoniae is a common source of bacterial infections in children, the elderly and AIDS patients, says Tomasz. Scientists estimate this bacterium is responsible for up to 6 to 7 million middle ear infections in children, and about a half million cases of community-acquired pneumonia each year in the United States alone. Worldwide, the number of deaths from infections with this bacteria each year are similar to that of tuberculosis–3 to 4 million.
In a study of S. pneumoniae, Tomasz and MirjanaNesin, M.D., found a multidrug-resistant form of the 23F strain that had switched its outermost coating, the capsule, to that of a S. pneumoniae 14 strain. Nesin plans to discuss the research at the Pediatric Academic Societies’ Annual Meeting on May 10 in Washington. D.C. She is associated with the Perinatology Center at Cornell University Medical Center and is a guest investigator at Rockefeller in Tomasz’s laboratory.
While the bacteria in their study came from one child’s throat, the scientists also found evidence of similar capsular switches involving the same 23F multidrug-resistant strain among isolates from people in New York City and from hospital patients in South Korea. In these cases, the bacteria appeared to adopt capsules of either the S. pneumoniae 9 or 19 strains.
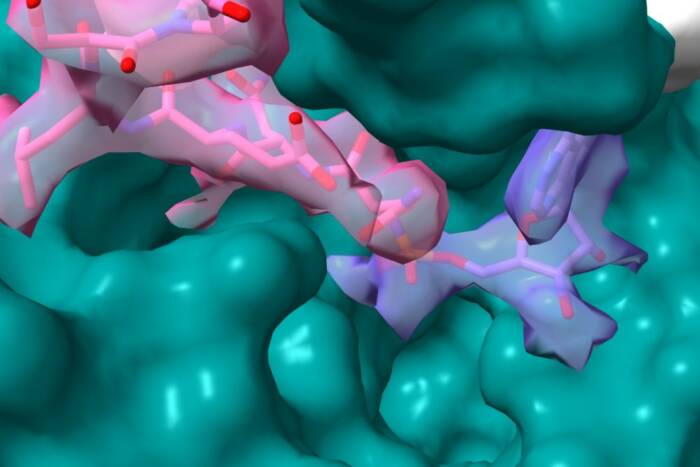
Switching capsules is important, Tomasz explains, because it could provide the bacterium with a temporary, protective disguise to hide from antibodies, the infection-fighting proteins made by the immune system. Antibodies are tailored to precisely match the capsule of each pneumococcal strain, so antibodies for one kind of capsule do not attach to another. Immune cells recognize and destroy bacteria tagged with antibodies.
In the study, Tomasz and Nesin used DNA sequencing and fingerprinting, laboratory techniques that examine the molecular structure of genetic material, to analyze drug-resistant genes in two pneumococcal isolates recovered from the throat of a child attending a U.S. day care center.
One of these isolates, with a type 14 capsule, was susceptible to all antibiotics. The second isolate was the 23F bacterium resistant to six antibiotics: chloromphenicol, erythromycin, penicillin, third-generation cephalosporin, tetracycline and sulfa-trimethoxazole. Tomasz and his colleagues first described these bacteria in a 1995 collaborative study with Frederick Henderson, director of the Department of Pediatrics at the University of North Carolina, Chapel Hill.
After a few weeks, the scientists found in the same child type 14 pneumococcal bacteria resistant to the same antibiotics as the previously identified 23F multidrug-resistant strain.
On closer examination, the scientists discovered that this multidrug-resistant 14 strain shared several characteristics with the resistant 23F strain. Both strains had identical surface proteins that bind to penicillin (PBP), the same DNA sequences of PBP 2X and 2B genes, and an identical overall chromosomal pattern.
“Only the capsule differed between the two strains, strongly suggesting the multidrug-resistant strain with the type 14 capsule is, in fact, a disguised version of the 23F multidrug-resistant bacterium. The 23F strain had switched its outermost coating,” says Nesin.
The most likely mechanism for the capsule switch, Nesin and Tomasz suggest, is that the multidrug-resistant 23F bacteria took genes from the drug-susceptible 14 strain during their common residence in the child’s throat. This gene-stealing process is scientifically known as transformation. With the help of the imported genes, the 23F bacteria then surrounded themselves with new coatings.
In related research, Tomasz and his colleagues have used DNA fingerprinting to document the spread of the multidrug-resistant 23F strain over large geographic distances, including several day care centers and hospitals in the United States, Spain, Portugal, Croatia and Korea.
In 1993, the U.S. Centers for Disease Control and Prevention (CDC) reported resistance to penicillin among more than 40 percent of pneumococcal bacterium identified from throat samples of children in Atlanta younger than six years. Similar or even higher rates of these resistant pneumococci were reported from Spain, Hungary, Japan and Korea, Tomasz notes.
Of historic note, scientists at Rockefeller in the 1940s explored the capacity of S. pneumoniae to undergo genetic transformation. These studies led to the discovery that genes are made of DNA(opens in new window), reported in 1944 by Rockefeller investigators Oswald T. Avery, M.D., Colin M. MacLeod, M.D., and Maclyn McCarty, M.D., inThe Journal of Experimental Medicine.
Tomasz’s laboratory receives funding from the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health. Also, grants from The Aaron Diamond Foundation, The Bodman Foundation and The Achelis Foundation helped support the research. Tomasz’s laboratory also is a center for a recently formed New York City initiative, the Bacterial Antibiotic Resistance Group, that uses molecular fingerprinting methods to track antibiotic-resistant bacteria in the hospitals in the metropolitian area.
Tomasz’s laboratory receives funding from the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health. Also, grants from The Aaron Diamond Foundation, The Bodman Foundation and The Achelis Foundation helped support the research. Tomasz’s laboratory also is a center for a recently formed New York City initiative, the Bacterial Antibiotic Resistance Group, that uses molecular fingerprinting methods to track antibiotic-resistant bacteria in the hospitals in the metropolitian area.