Metabolism protein found to also regulate feeding behavior in the brain
The molecular intricacies of hunger and satiety, pivotal for understanding metabolic disorders and the problem of obesity, are not yet fully understood by scientists. However, new research from The Rockefeller University reveals an important new component of the system responsible for regulating food intake: a hormone called amylin, which acts in the brain to help control consumption.
“How much a person eats is regulated by a complex circuit, and in order to understand it, we need to identify all the molecules involved,” says Jeffrey Friedman, Marilyn M. Simpson Professor and head of the Laboratory of Molecular Genetics at Rockefeller. “Amylin caught our attention when we were profiling a set of neurons in the hypothalamus, a part of the brain known to be involved in feeding behavior. Because it plays a role in sugar metabolism elsewhere in the body, we were interested in exploring its function in the brain.”
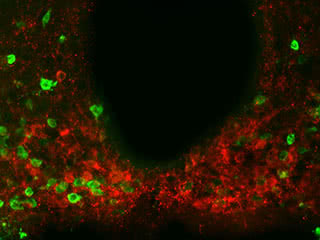
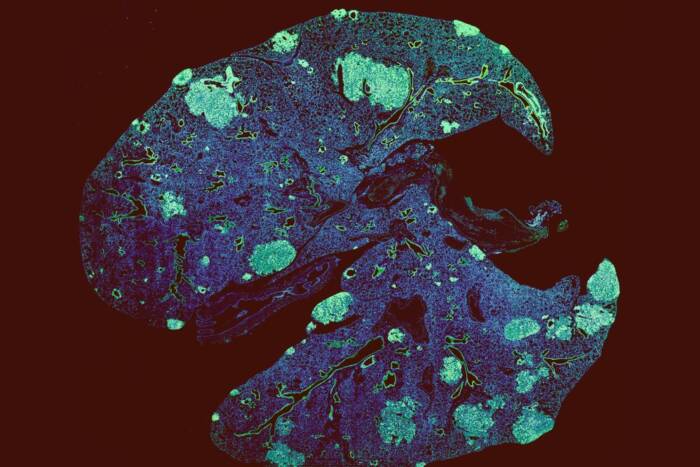
Curb your appetite: Scientists found evidence of the metabolism-regulating protein amylin, shown in red, present in multiple regions throughout a brain area called the hypothalamus. Experiments suggest amylin produced by hypothalamic neurons helps reduce food consumption together with leptin.
What stops us from eating too much?
Friedman is well-known for his 1994 discovery of the hormone leptin, one regulator in this process. Defects in leptin production are associated with obesity. However, treating obesity with leptin alone has not proven effective except in cases of severe leptin deficiency, suggesting that additional components are involved in this system.
The findings, published recently in Cell Metabolism, suggest that leptin and amylin work in concert to control food intake and body weight.
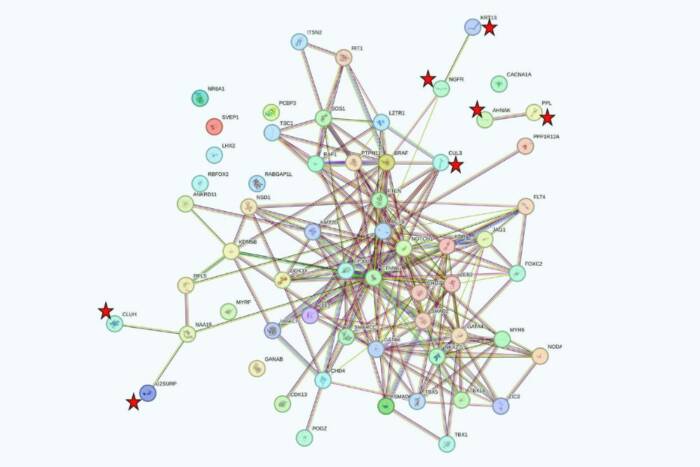
Friedman and colleagues first identified the precursor to amylin—called Iselt amyloid peptide (Iapp)—in the brain by using a technology known as translating ribosome affinity purification, previously developed by fellow Rockefeller scientists. The researchers found that Iapp is abundant in multiple regions throughout the hypothalamus. (Incidentally, these findings contradict previous results, suggesting that prior experiments, which have not consistently found amylin in the brain, may not have used techniques sensitive enough to detect Iapp.)
To tease out the function of amylin in the hypothalamus, the researchers assessed its presence in mice that were obese due to leptin deficiency. When these mice were given leptin, their Iapp levels increased significantly, indicating that leptin regulates the expression of amylin.
Molecular teamwork
“We also looked directly at how amylin and leptin affect feeding behavior,” says lead author Zhiying Li, a research associate in the lab. “When we give leptin to mice, it significantly suppresses food intake. However, when we give leptin to mice in which amylin is rendered nonfunctional with an inhibitor, the effect of leptin is blunted. This means that leptin and amylin are working together in a way that reduces feeding.”
Additionally, the researchers evaluated how amylin controls neural signals. From recordings of neuron signals showing that leptin and amylin act on the same neurons in similar ways, they hypothesize that these hormones act in a synergistic manner, working together to produce an enhanced neural signal.
“These findings confirm a functional role for amylin in the central nervous system, and provide a potential mechanism to treat obesity more effectively, through combination therapy,” says Friedman. “While this is a piece of the puzzle, we still need a better understanding of the cellular mechanisms involved in this system, which could provide new approaches that involve improved leptin signaling and sensitivity.”
This work is supported by funding from The JPB Foundation.
 Cell Metabolism 22, 1059–1067 Cell Metabolism 22, 1059–1067Hypothalamic Amylin Acts in Concert with Leptin to Regulate Food Intake Zhiying Li, Leah Kelly, Myriam Heiman, Paul Greengard, and Jeffrey Michael Friedman |