Daniel Mucida, who studies the gut’s specialized immune system, receives promotion
Daniel Mucida’s research focuses on how the intestinal immune system balances vigilance to threats with tolerance to harmless foreign proteins.
As of September 1, Daniel Mucida, who heads the Laboratory of Mucosal Immunology and studies the immune system along the vast surface of the intestine, will become an associate professor. The Board of Trustees approved his promotion on July 29.
Although hidden from view, the gut has more interaction with the outside world than any other part of the body. Covering an expanse much greater than the skin, the intestinal lining comes in contact with every meal we ingest. The gut also has its own ecosystem of trillions of resident microbes. As a result, it offers a unique place to study how the body decides when to tolerate a foreign element and when to go on the defensive.
“The intestine is home to more immune cells than any other part of the body,” Mucida says. “Our lab studies how cues from their locations within its lining prompt these cells to promote an inflammatory response to a potential danger, or to calm inflammation to prevent self-inflicted damage.”
Since he arrived at Rockefeller in 2010, Mucida has pushed his study of this remarkable aspect of human biology into new and fascinating directions, including, for instance, how neurons and immune cells communicate within the gut, says Marc Tessier-Lavigne, the university’s president.
“An emerging leader in his field, Daniel is an energetic and creative scientist who has built a thriving laboratory at Rockefeller,” Tessier-Lavigne says. “His work has important implications for immunological, infectious, and even neurological diseases.”
The thin boundary and below
Many factors set the gut apart from other organs: It has a massive surface area, estimated to cover about 300 square meters, a bit larger than a doubles tennis court. Food, and the foreign proteins within it, continually passes through the interior, or lumen, of the intestine, where most of the body’s resident microbes—its microbiome—is found.
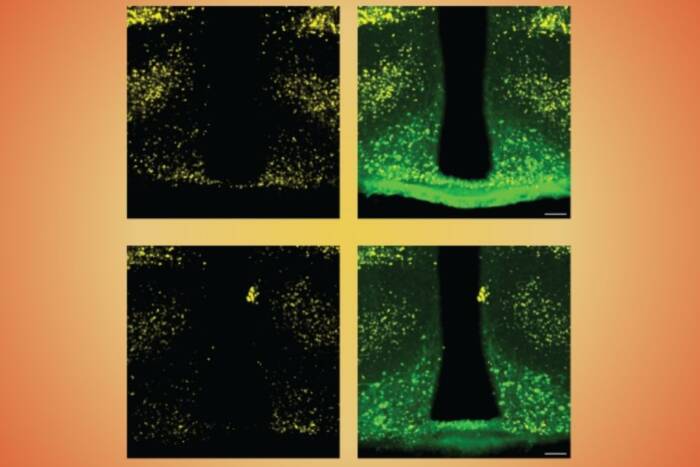
The outer layer of the intestine’s lining, a thin boundary of epithelial cells, allows nutrients to flow in—and it also creates opportunity for pathogens to invade. Much of the work in Mucida’s lab concentrates on one specialized class of immune cells, known as intraepithelial lymphocytes (IELs), which inhabit the space just below the epithelial layer and sometimes move within it.
IELs, a type of T cell, can help calm the inflammatory response. In recent research, Mucida and colleagues explored how cues from the epithelium, including the presence of microbes, can induce other T cells to become IELs. His lab wants to better understand how IELs help the immune system tolerate foreign proteins in food, and how they patrol the epithelial layer to protect the body against pathogens.
Move a little deeper into the gut, between the first two layers of muscle, and you’ll find a space containing, among other things, a network of neurons as well as more immune cells. Because neurons communicate via electrical signals, Mucida’s lab works with a hypothesis that they might provide a means for quickly syncing immune activity across a large area.
His recent work has shown that, during infection, these intestinal neurons send calming signals to large invader-eating immune cells called macrophages, helping to prevent excessive inflammation. Much remains unknown about the relationship between gut’s neurons and its immune system, and a key focus of Mucida’s work moving forward will be to study their interactions in more detail.
Beyond the gut
Another area of inquiry focuses on a phenomenon that begins in the gut, but has far-flung effects. In theory, every foreign protein we eat has the potential to cause a major allergic reaction; a phenomenon known as oral tolerance prevents this from happening. Mucida’s lab is exploring how signals from the gut travel to other parts of the body, preventing such overreactions.
His lab has found that a particular population of dendritic cells, a type of immune cell, migrates from the intestine into the lymphatic system, ultimately inducing the production of anti-inflammatory T-cells elsewhere in the body. He is now looking at other mechanisms by which interactions in the gut can calm immune reactions far away.
“Evidence connects gut reactions with a host of diseases that occur far beyond the gut, from autism to arthritis to allergies,” Mucida says. “My hope is that our research on immune regulation in the gut could have significant medical importance.
“I have been fortunate enough to recruit many talented and hardworking scientists,” he adds, “without whom my work would not be possible, and I look forward to continuing to collaborate with such a productive group.”