Study identifies genetic mutation responsible for tuberculosis vulnerability
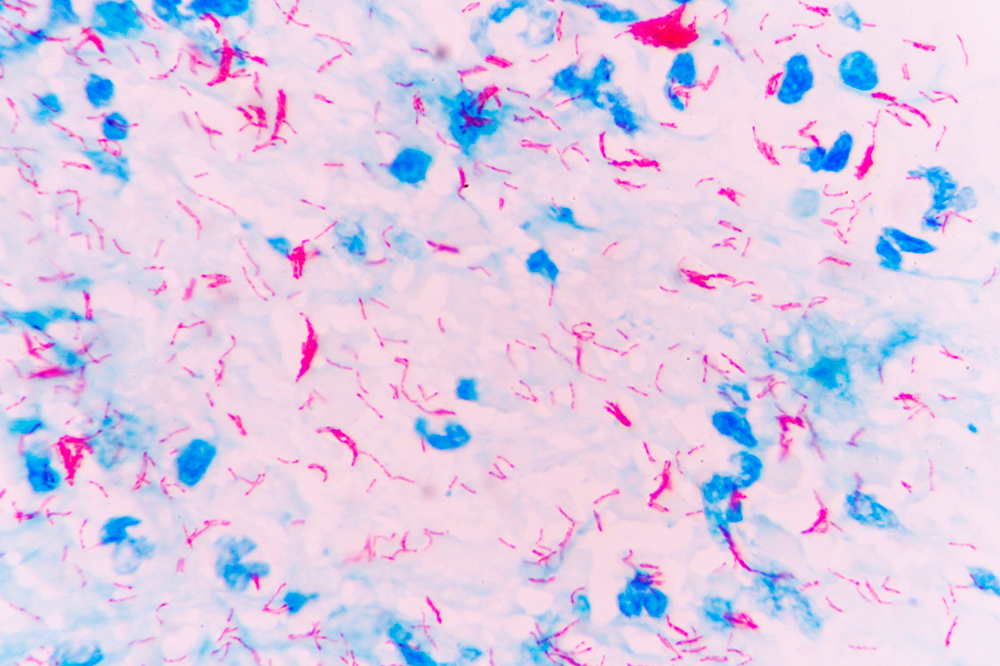
In some people, infection with the microbe Mycobacterium tuberculosis can lead to serious illness, and even death. In others it is harmless.
If you live in the United States, you are unlikely to come into contact with the microbe that causes tuberculosis. Your odds of encountering the microbe are so low, in fact, that risk factors for the disease can easily go unnoticed: If you happened to carry a gene that predisposed you to tuberculosis, you likely wouldn’t know.
New findings from Rockefeller scientists reveal that such a genetic variant indeed exists—and that it’s surprisingly common.
The researchers also uncovered genetic mutations that rob the immune system of its ability to combat more ubiquitous germs of the same bacterial family, mycobacteria. In two new studies, both published in Science Immunology, they elucidate molecular abnormalities that make people vulnerable to mycobacterial infections. This research also points to strategies for treating or preventing some cases of tuberculosis (TB).
The most common mutation you’ve never heard of
About one in five people worldwide are infected with Mycobacterium tuberculosis, the bacterium that causes TB. Of those, only 10 percent, at most, will show symptoms—because most immune systems have tools to fight the microbe. When these tools are absent or dysfunctional, however, the infection can damage the lungs and other organs, and even cause death.
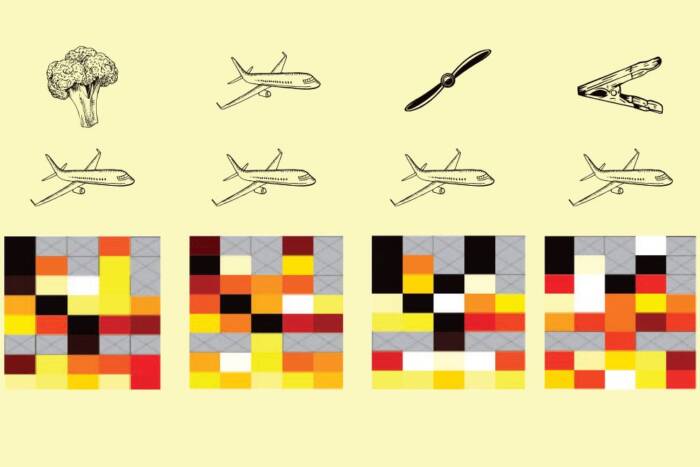
Hoping to better understand why only some people are prone to TB, Jean-Laurent Casanova worked with clinicians across the world to collect DNA samples from patients with active forms of the disease. By analyzing these samples, the researchers discovered that the risk of developing TB is heightened in people who have two copies of a particular variation to the gene coding for the enzyme TYK2. Moreover, the researchers found, this genetic condition is fairly widespread.
“In Europeans, one in 600 people have two copies of this TYK2 variation. And in the rest of the population the rate is between one in 1,000 to one in 10,000—which is still not rare,” says Casanova. Putting these numbers in perspective, he adds: “Here at Rockefeller, there are probably around four to six people who have this genetic predisposition to TB.” Yet, that is not to say that those people will actually develop the disease—and, in fact, they probably won’t.
Put simply: People don’t acquire TB if they don’t come into contact with Mycobacterium tuberculosis. And in the United States and Europe, the risk of being exposed to the microbe is very low. As a result, a New Yorker with a TYK2 mutation might never find out that she is genetically vulnerable—that is, unless she travels to a location where the microbe is rampant.
Says Casanova: “In New York, someone can have this mutation and their risk of getting TB is effectively zero. But if that person goes to work in a TB hospital in Africa, then the likelihood of getting TB is high—one hundredfold higher than it would be for a person without the genetic variant.”
Historically, a person with a TKY2 mutation would be unaware of her susceptibility until it was too late. However, now that researchers have identified this risk factor, individuals travelling to regions where TB is common can obtain genetic tests to find out whether they are vulnerable to the disease.
Immunological insight
Mycobacterium tuberculosis belongs to a broader class of microbes known as mycobacteria. Most of these germs are ubiquitous, but harmless.
“These are bacteria that are in tap water, or in your sandwiches. They’re everywhere,” says Casanova. “But most of them are poorly virulent—they’re weak, compared to Mycobacterium tuberculosis—so in the vast majority of people, they’ll never cause disease.”
In a small fraction of the population, however, these common microbes can lead to serious infections—a condition known as Mendelian susceptibility to mycobacterial disease, or MSMD. Recently, Casanova and his colleagues identified two novel genetic causes of this condition, one that leads to a deficiency of the receptor for the immune cell protein IL-23, and one that leads to a deficiency of the receptor for a similar protein, IL-12.
Both IL-12 and IL-23 promote production of gamma interferon, a molecule that contributes to immunity against mycobacterial infections. When cells fail to produce this interferon at normal levels, they become susceptible to widespread, poorly virulent mycobacteria. In other words, they develop MSMD. The risk for this condition is highest, the researchers found, among individuals with a mutation that affects both IL-12 and IL-23 receptors.
“Though the two proteins are individually important, their function is somewhat redundant. So most people missing only IL-12 or IL-23 will be ok, only some of them developing MSMD,” says Casanova. “But if you lack both, then you have very low interferon production and will almost certainly develop the condition.”
In addition to elucidating a new genetic cause of MSMD, this research helped the scientists understand why a TYK2 mutation might make people prone to TB. They found that when the enzyme’s function is disturbed, cells don’t respond normally to IL-23, and therefore produce less gamma interferon. And though low interferon levels may suffice to stave off poorly-virulent bacteria, they do not protect against stronger microbes like Mycobacterium tuberculosis.
This finding, says Casanova, suggests a new strategy for treating people with TB.
“What IL-23 does for a living is induce gamma interferon, which, it turns out, you can buy at the pharmacy,” he says. “So if you’re prone to TB because of a mutation to TYK2, you could potentially prevent or treat it with that kind of medicine.”