Dendritic cells may be key to reversing diabetes
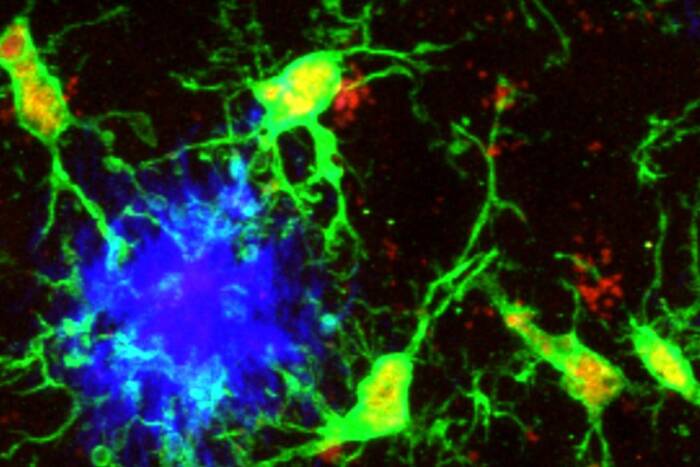
When the body’s own immune system begins to assault the cells in the pancreas responsible for producing insulin, the result is type 1 diabetes. Now, researchers studying the immune system’s dendritic cells in mice have found a way to stop the destruction and help revive and maintain the population of insulin-producing β cells, a discovery that could lead to a lasting cure.
In two closely linked papers, Rockefeller University scientists have shown that they can use dendritic cells in two different capacities to restore normal function to diabetic mice. Dendritic cells direct the body’s immune response by stimulating other immune cells and expanding them. By exploiting their ability to regulate the actions of rogue immune responses, the researchers found they could halt the course of the disease.
A study published in the Journal of Experimental Medicine by Henry G. Kunkel Professor Ralph Steinman, head of the Laboratory of Cellular Physiology and Immunology, and first author and research associate Kristin Tarbell, shows that dendritic cells can be used to help boost the number of regulatory T cells, which help protect β cells from destruction. The scientists gave diabetic mice regulatory T cells that had been expanded by dendritic cells. They found that the treatment restored normal blood sugar regulation to about half of the mice – essentially curing their diabetes. What’s more, the immune systems of the successfully treated mice continued to expand the regulatory T cell population, helping prevent further β cell attacks.
In the second study, published in the Proceedings of the National Academy of Sciences, Steinman and Tarbell, together with their colleagues Xunrong Luo at Northwestern University and Manikkam Suthanthiran at Weill Medical College of Cornell University, show that dendritic cells can also be used in conjunction with islet cell transplants, a procedure sometimes used to treat diabetic patients. Using dendritic cells and a growth factor called transforming growth factor β, the scientists prodded the naïve T cells to differentiate into the β cell-protecting regulatory T cells. This process allows an increase in the numbers of the normally rare regulatory T cells. Then, the researchers grafted insulin-producing islet cells into non-obese diabetic mice — a procedure that’s being developed for human diabetes patients, who must then take immunosuppressive drugs to maintain the graft. But the new regulatory T cells, deposited at the site of the graft, protected the islet cells without the need for immunosuppressive drugs.
“Everything we’ve done so far is in the mouse model, but we’re very interested in translating it into humans,” Tarbell says. “We have a long way to go before that happens. But just as an example, we hope that someday it’ll be possible to take out dendritic cells from a patient, culture them with islet cells, and use the dendritic cells along with a growth factor to stimulate a regulatory T cell population. Then you could put the regulatory T cells back into people to treat them.”
Journal of Experimental Medicine 204(1): 191-201 (January 22, 2007)(opens in new window)
Proceedings of the National Academy of Sciences 104(8): 2821-2826 (February 20, 2007)(opens in new window)