HIV-1 kills immune cells in the gut that may never bounce back
People with HIV have been living longer, healthier lives since the development of highly active antiretroviral therapy (or HAART) in 1995. In fact, most patients on the drug regimen do so well that, according to blood tests, their immune cells appear to return to pre-HIV levels. But two new studies from Rockefeller University and the Aaron Diamond AIDS Research Center show that within the gastrointestinal tract, recovery of immune cells is incomplete despite years of prolonged treatment, suggesting the need for additional ways to monitor immune system health, and the need for hypervigilance as HIV-positive patients live into their forties, fifties, sixties and beyond.

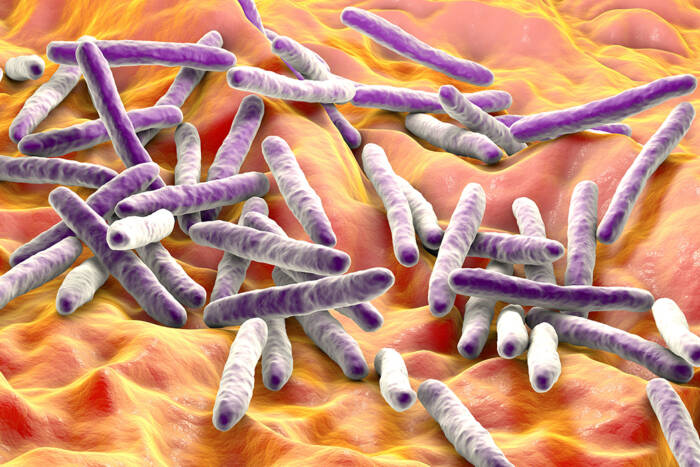
Gut-wrenching news. People with healthy immune systems have a large reservoir of immune cells known as CD4+ memory T cells (dark pink spots) in their GI tracts, many of which are killed off after infection with HIV-1. New research shows that even after two or more years of intensive antiretroviral drugs, that population of immune cells does not return.
Prior research had shown that, just two to four weeks after contracting HIV-1, the lymphoid tissue layer in the mucous membrane of a patient’s gastrointestinal (GI) tract can lose up to 60 percent of its CD4 memory T cells — immune cells responsible for recognizing invaders and priming other cells for attack. Intrigued, Martin Markowitz, an Aaron Diamond Professor at Rockefeller University and a staff scientist at the Aaron Diamond AIDS Research Center, wanted to know whether this loss was reversible, and whether giving patients HAART during the early infection period would help restore these cells to the GI lining the way it restores them to the blood itself.
In a paper published today in PLoS Medicine, Markowitz, Rockefeller researcher and clinical scholar Saurabh Mehandru and their colleagues report on a trial of 40 HIV-1-positive patients who began treatment with HAART shortly after contracting the virus — during the acute early infection phase — and who they followed for one to seven years. The researchers found that although the blood population of CD4 T cells rebounded to normal levels, a subset of the GI tract population remained depleted in 70 percent of their subjects. “If we sample the blood, it only has two percent of the total volume of these cells. It doesn’t give us the whole picture,” Markowitz says. “But if we actually go into tissue, we see something different. What we see there is eye-opening.” After three years of intensive drug therapy that suppresses HIV replication very effectively, most patients still had only half the normal number of CD4+ effector memory T cells in their GI tracts.
“Obviously the first question is, why? What’s the mechanism?” Markowitz asks. A second paper, published online in the Journal of Virology, makes some headway toward an answer. By examining the viral burden of DNA and RNA in cells from the GI tract, and comparing that to cells from the peripheral blood, Markowitz, Mehandru and their collaborators determined that the mucosal lining of the GI tract carried a disproportionately heavy viral load. That means that the initial loss of CD4 T cells in that area is partially due to virus activity. But the researchers also found evidence suggesting that there are at least two more ways in which the cells were being killed off. Some of the T cells self-destruct (a process called activation-induced cell death or apoptosis), while some appear to be killed by other cytotoxic immune cells. “These papers speak strongly to HIV pathogenesis, to HIV therapy and to understanding how the host and virus interact,” Markowitz says. However, the short- and long-term consequences of the persistence of this depletion remain unknown.
In the clinic, if the loss of CD4 T cells in the GI tract translates into increased incidence of colonic polyps or colorectal cancer, routine monitoring practices will have to be re-examined, with HIV-positive patients receiving colonoscopies earlier and perhaps more frequently than current recommendations allow. Markowitz says. “It’s pretty clear that a successful vaccine will need to address issues surrounding mucosal immunity, which is an area that — relatively speaking — has been previously ignored.”
PLoS Medicine 3(12): e484
Journal of Virology Online: October 25, 2006