The blood may hold clues to some of COVID-19’s most mysterious symptoms
Erin Norris and Pradeep Singh discuss their research in the laboratory of Sidney Strickland.
The most severe cases of COVID-19 begin with leaky blood vessels. Breaches in the vascular system cause inflammation and coagulation, as fluid floods the lungs. Meanwhile, a host of seemingly unrelated symptoms set in. Blood pressure drops, arrhythmias test the heart, and the central nervous system takes a beating.
Some studies suggest that such disparate symptoms may have a single culprit—a tiny molecule known as bradykinin—and scientists now suspect that SARS-CoV-2 is capable of toppling the delicate system that keeps this signaling substance in check. The result is a runaway bradykinin storm, the hallmarks of which just happen to be inflammation, blood coagulation, and heart, lung, and brain complications.
Rockefeller’s Sidney Strickland knows a thing or two about bradykinin, having studied it at length in the context of neurodegenerative diseases, inflammation, and blood coagulation. His lab was the first to demonstrate that the β-amyloid peptide, thought to cause Alzheimer’s disease by forming sticky plaques in the brain, also sets in motion a cascade of molecular events leading to the release of bradykinin, a likely cause of inflammation and coagulation in Alzheimer’s. Strickland’s pursuit of this relatively uncelebrated cascade may explain why vascular problems often crop up in neurodegenerative conditions.
So when COVID-19 began presenting not as a straightforward infection but a complex systemic disease—complete with the telltale signs of a bradykinin storm—the Strickland lab was ready.
“When we began looking into COVID-19, our first thought was that the inflammation characteristic of severe cases might be coming from the plasma contact system,” says Erin Norris, a research assistant professor in Strickland’s lab. The plasma contact system works by activating a plasma protein known as Factor XII, which triggers coagulation and, along the way, releases bradykinin to induce inflammation. “By investigating the plasma contact system, we can study inflammation and coagulation all at once,” she says.
A promising hypothesis
The first step for the Strickland lab is demonstrating that the novel coronavirus does indeed set off a bradykinin storm—a theory that matches the sundry symptoms but remains unproven.
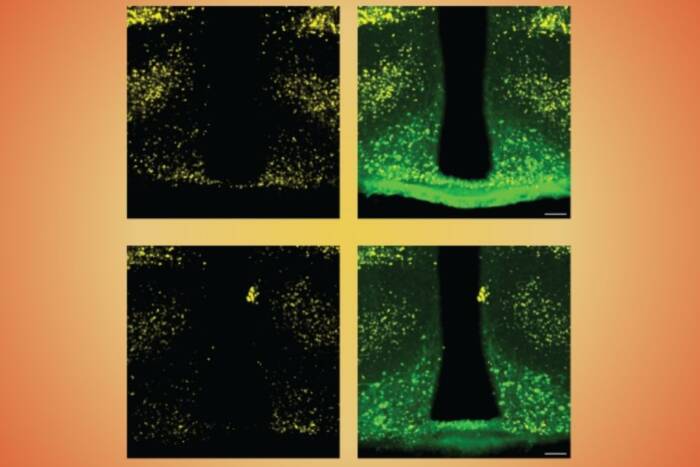
Because research on a dangerous pathogen like SARS-CoV-2 requires extreme safety precautions, the lab is testing the idea using a faux coronavirus, developed in the lab of Paul Biensiasz, that is less cumbersome to work with than the real pathogen. By observing how the faux coronavirus interacts with plasma samples in the lab, scientists can determine whether the artificial virus does indeed set off a bradykinin storm by way of the contact system. If confirmed, the implications for clinicians managing severe COVID-19 cases could be imminent.
“There are existing medications that block the contact system and inhibit the production of bradykinin without interfering with the body’s main clotting pathways,” Norris says.
In a separate set of experiments, Strickland’s lab is also analyzing plasma samples from COVID-19 patients in various stages of the disease. They’re hoping to find a correlation between the severity of symptoms and the level of contact system activation since there is currently no way for doctors to predict which newly infected patients are at risk of developing life-threatening disease. If, for example, it turns out that the plasma contact system goes into overdrive before a patient takes a turn for the worse, clinicians could use this information to identify severe cases early on.
“We could create a test to determine the extent of contact system activation and use it to identify which patients are most likely to experience coagulopathy or inflammation,” Strickland says. “If certain patients are more likely to develop serious problems, it would be great to know this early on so approved medications could be employed.”
Although the research is still in its early stages, the plasma contact system is an increasingly appealing target in the fight against COVID-19. “Something is leading to coagulation and inflammation,” Strickland says. “The contact system is promising because it can do both.”