Aggravated assault: How adhesion proteins regulate skin inflammation
When it comes to skin, the tighter the better. To create an effective barrier, cells in the epidermal, or outermost, layer of the skin form very tight associations. But while strong links between skin cells protect the body from the world outside, new research from Rockefeller University shows that the proteins that create these bonds are also key components of a pathway that prevents rampant inflammation.
 (opens in new window)
(opens in new window)
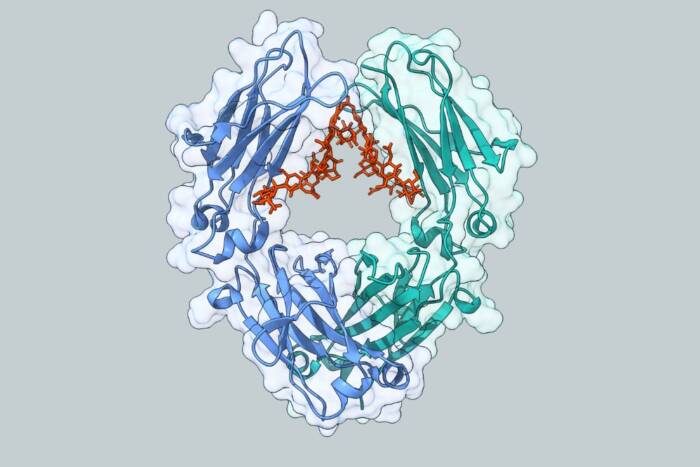
Skin tight. To maintain the tight connections needed to protect the body’s inner organs, skin cells use the protein E-cadherin (green) to connect to one another. But when proteins involved with E-cadherin’s function are missing, the cell’s structural cytoskeleton (red, above) rearranges into stress fibers, inhibiting its normal pattern. These same proteins have now been identified as key components of a pathway that prevents rampant inflammation.
Inflammation occurs when skin cells recruit immune cells to help fight infections. As a response to injury and foreign invaders it’s a healthy, even critical function. But unchecked it can spin out of control, leading to chronic inflammatory diseases, as well as cancers.
In a series of papers published this month, Elaine Fuchs, head of Rockefeller’s Laboratory of Mammalian Cell and Developmental Biology, has shown that two of the proteins, called catenins, that help adhere skin cells to one another at the junctions where they come together, are also essential for maintaining control of the inflammation pathway. There are actually three types of catenin proteins in skin cells, known as alpha-catenin, beta-catenin and p120-catenin. When the gene for either alpha-catenin or p120-catenin is deleted, the cells in the skin go down a road of hyperproliferation and/or super-inflammation, leading to a number of chronic skin conditions.
“It is extraordinary that the loss of either one of these proteins, previously thought to be strictly involved in cell-cell adhesion, can account for so many changes in both skin architecture and function,” says Fuchs, a Howard Hughes Medical Center investigator.
Scientists in Fuchs’ lab bred mice missing the gene for either alpha-catenin or p120-catenin, but only in the epidermis. The effects they saw shared some similarities – their internal skeletons, called a cytoskeleton, were rearranged and the mice were found to have raised levels of a nuclear protein cell NFkB, a pro-inflammatory protein that when transported into the nucleus, promotes activation of other inflammatory genes. In the case of p120-catenin, lead author Mirna Perez-Moreno, a postdoc in the Fuchs lab, found that a small protein called RhoA was the link. “Rho proteins act as molecular switches that can be activated to regulate the cytoskeleton,” says Perez-Moreno. “But they also have an impact on other aspects of cell behavior, including the regulation of NFkB activity.”
In both the p120-catenin and alpha-catenin cases, “The initial signal comes from the epidermis,” explains Perez-Moreno. “But then the inflammatory cells are recruited and they start secreting more inflammatory proteins, which then activate other receptors on the epidermal cells. This response amplifies the inflammatory pathway and can transform it into a chronic inflammatory event.”
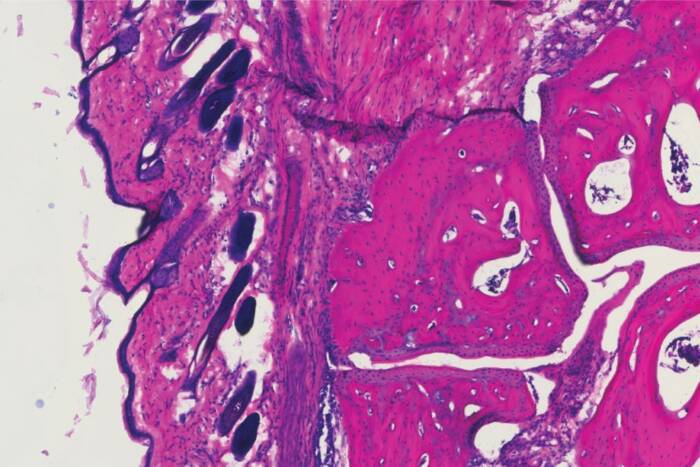
The effects were compounded in skin without alpha-catenin because the epidermis completely lost its ability to maintain adherens junctions between cells, something that didn’t happen in the mice missing p120-catenin. In addition, when the alpha-catenin gene was missing, the cells in the alpha-catenin-deficient skin divided out of control. This situation in humans is very similar to squamous cell carcinoma, one of the most common cancers worldwide. Agnieszka Kobielak, another postdoc in the Fuchs lab and lead author on the alpha-catenin story, examined tissue taken from over 30 different human skin cancer patients with squamous cell carcinomas, and found that the majority of them have reduced alpha-catenin, raised levels of NFkB, and inflammatory cells in the dermis.
Because tissues with chronic wound and inflammatory diseases are known to be more susceptible to cancer, Fuchs and colleagues hope that a better understanding of each protein’s contribution to the inflammation response will help identify specific targets for anti-inflammatory treatments that may also help prevent cancer. “A connection between inflammation and cancer has been suspected for decades,” says Fuchs, “but we are just now beginning to understand that it is as much a prerequisite as a consequence of tumorigenesis.”
Cell 124: 631-644 (February 10, 2006)(opens in new window)