Genetic 'stress response' may explain how bacteria resist drugs
Antibiotics are great, when they work. Unfortunately, bacteria have a nasty habit of developing resistance to even our most powerful pharmaceuticals. Now, by tracking the staph infection of a single patient during a course of antibiotic treatment, Rockefeller University scientists have discovered new clues to how bacteria evolve to be able to resist drugs.
Staph infections, caused by the Staphylococcus aureus bacteria, are a particular plague on hospitals, and increasingly doctors are finding that staph are resistant to even their drug of last resort, vancomycin.
“Previous studies have tried to characterize the mechanisms for vancomycin-resistance,” says Rockefeller’s Alexander Tomasz, the senior author of the study, “but the major problem has been that no vancomycin-susceptible parental strain was available that could be used for comparison. In our study, we had access to isolates of S. aureusfrom a single patient at different times during vancomycin therapy, and this provided us with an opportunity to look at how the bacteria change over time in response to antibiotic treatment.”
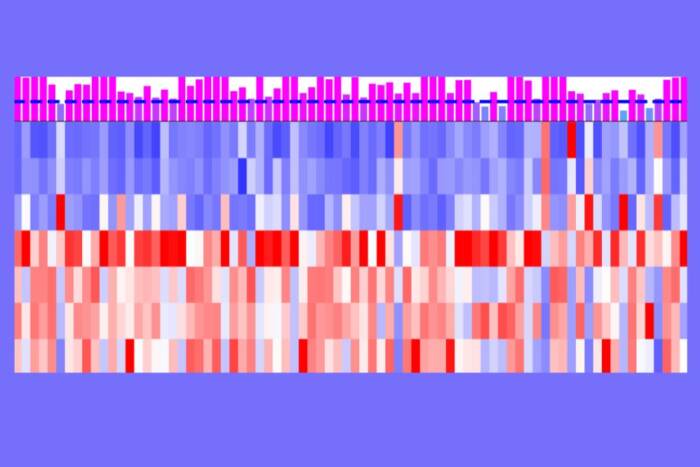
Using custom-designed gene chips, Tomasz and colleagues compared samples of S. aureus bacteria from the patient, taken at different times during treatment, looking for variations in their genetic blueprints. Their experiments confirmed that both the resistant and the susceptible parental bacteria were isogenic, meaning they carried the same genetic determinants.
The scientists then turned their attention to how those genes were read in the drug-susceptible isolates, as compared to the drug-resistant ones. A surprisingly large number of genes showed abnormal activity — over-expression or repression — in the resistant cells, and many of the over-expressed genes belonged to proteins involved with the synthesis of staphylococcal cell walls, unsurprising since vancomycin kills bacteria by targeting their cell wall.
Further research showed that not only did these genes turn on when the bacteria were first exposed to antibiotic treatment, they remained stuck in the on position in the resistant cells. Susceptible bacteria treated with vancomycin respond by activating genes involved in their stress response. These same genes are active in the resistant bacteria too, even without any antibiotic present.
“The mechanism of this type of vancomycin resistance seems to involve the permanent fixation of a stress response in the genome of the resistant bacteria,” says Tomasz. Understanding the mechanisms that the bacteria adopt to survive may help scientists in the design of future drugs and treatments against the threat of antibiotic-resistant bacteria.
Journal of Bacteriology 188(3): 1120-1133 (February, 2006)(opens in new window)