Building a better vaccine
Rockefeller’s Charlie Rice thinks that scientists struggling to create a vaccine to protect against the widely predicted avian flu pandemic might learn a thing or two from yellow fever.
“The yellow fever 17D vaccine is one of the most successful vaccines ever created,” says Rice, the Maurice R. and Corinne P. Greenberg Professor and head of the Laboratory for Virology and Infectious Disease. “Surprisingly, though, how it elicits such a robust immunity has never been addressed.”
But by studying how the yellow fever vaccine creates a potent, lifelong immunity after a single shot, Rockefeller scientists say they could unlock secrets that will help design new vaccines to target not only the influenza virus, but perhaps other infectious diseases such as HIV or hepatitis C. In a new paper published this month in the Journal of Experimental Medicine, Rice and his colleagues demonstrate one mechanism by which the vaccine does its job: by infecting specific cells in the immune system, they say, the inoculation promotes an unexpectedly robust immune response.
Yellow fever is a deadly virus, most common in the tropical areas of Africa and South America, which causes hemorrhage, multiple organ failure and is lethal in 20 to 50 percent of all cases.
“The characteristics of yellow fever make it tricky,” says Randy Longman, co-first author and a biomedical fellow in Rice’s lab. “With infectious diseases, you want to develop a mouse model of how the disease works. But yellow fever doesn’t infect mice the same way it infects humans, so we have to gather data using humans to understand how the virus works.”
Though many vaccines use dead forms of the virus, the yellow fever 17D vaccine, developed at the Rockefeller Institute in the 1930s, uses a live, but weakened, form of the virus that differs from the normal virus by just 32 amino acids out of thousands.
To develop immunity to yellow fever, only a single shot is needed. After one application, both major immune cell types, B and T cells, are primed to fight a repeat infection. Rice and colleagues wanted to know why the 17D vaccine was so effective, specifically how it initiates such a strong immune response. Once that is known, similar principles could be applied to future vaccine development.
“It is clear that for many types of infection, the T cell response plays a key role,” says Longman. “And we know that even decades after immunization, a person maintains immunity to a yellow fever infection. Understanding how the YF17D vaccine does that is really important.”
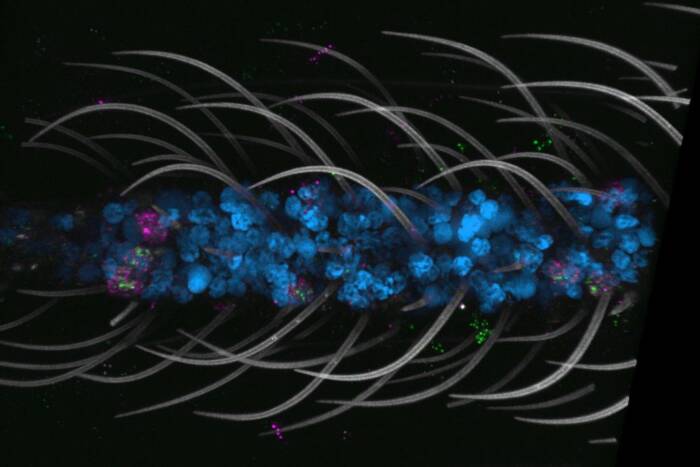
The researchers started with dendritic cells, which play a crucial role in the activation of T cells. By showing T cells parts of viruses or bacteria, dendritic cells stimulate T cells and then send them out on a mission to “find and destroy” any infected cells. Based on previous studies on other viruses, Rice and colleagues hypothesized that their yellow fever vaccine was directly infecting dendritic cells.
They found that the vaccine could infect both immature and mature human dendritic cells. The virus kills the immature dendritic cells, but mature dendritic cells, which interact with T cells, are able to process the virus and then present it to T cells to activate them.
Rice and colleagues then went one step further. They placed an influenza gene within the DNA of the yellow fever vaccine, and found that dendritic cells could present the inserted influenza protein fragment to activate T cells. Based on their finding, they conclude that the modified yellow fever vaccine could be used to vaccinate people against more than one infectious disease.
“Although the vaccine has been used to vaccinate hundreds of millions of people worldwide, many people have not received the vaccine in parts of the worlds where the virus is not a threat,” says Longman. “Therefore there is still great potential to use this vaccine for wide vaccination.”
“Lots of time is spent studying diseases where we don’t have a good model for protective immunity,” says Rice. “The yellow fever vaccine gives us that model, but because it works, there has been very little money to study it. Now there are new initiatives supporting research in vaccine development and an understanding how the yellow fever vaccine works may help guide the design of better, more potent vaccines in the future.”
Journal of Experimental Medicine 202(9): 1179-1184 (October 30, 2005)(opens in new window)