What we need to worry about with avian flu—and what we don’t

Since it was first detected in birds in late 2021, avian flu has killed millions of poultry and infected animals that were previously thought to be immune, including dairy cows. The FDA has documented the H5N1 virus in animals in 48 states.
Yet only 27 people worldwide have been infected since the outbreak began, and only four have been in the U.S. That suggests the risk to humans remains relatively low—for now. Why? And what early warning signs could point to an increasing risk?
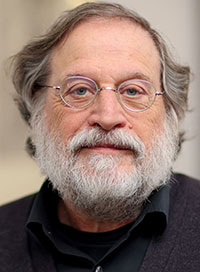
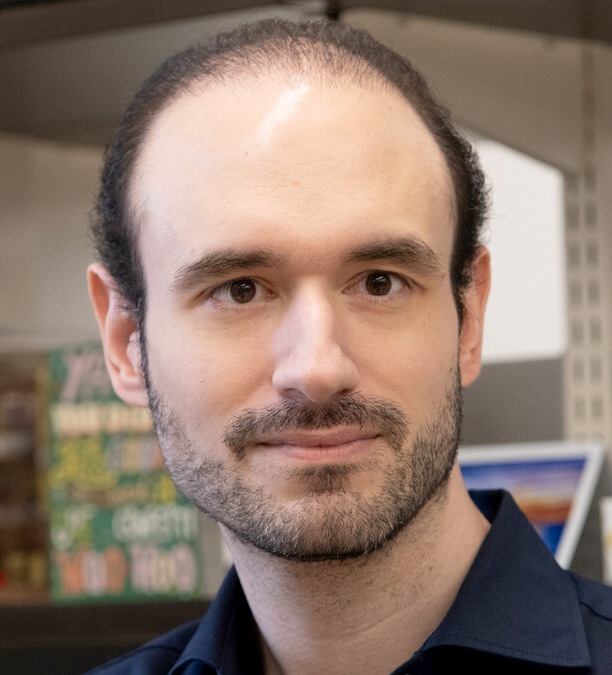
To find out, we spoke to Stylianos Bournazos, a research associate professor in the Leonard Wagner Laboratory of Molecular Genetics and Immunology at Rockefeller(opens in new window), headed by Jeffrey V. Ravetch. Part of a research consortium supported by the National Institute of Allergy and Infectious Diseases and the SNF Institute for Global Infectious Disease Research at Rockefeller, Bournazos and his fellow researchers have been tasked by both institutions with a crucially important project: the development of a universal influenza vaccine that protects against every flu strain—those currently circulating and any yet to emerge.
Let’s start with the big question. How worried should we be about avian flu?
The good news is that we’ve had only four human cases in the United States—farm workers in Texas, Colorado, and Michigan. Two of them only had mild cases of conjunctivitis, or pink eye, and the other two developed a cough, sore throat, or fatigue. Thus far, it doesn’t seem transmittable from person to person.
And the bad news?
The fact that the virus has acquired the ability to cross to different species. We’re primarily seeing cows infected. Again, largely with no or mild symptoms—but still the cows are a bit more worrying because we have a lot of animals in confined spaces near humans, and we don’t know exactly how the virus is being transmitted between the animals. We suspect it’s close contact.
Domestic cats on farms have died from drinking raw infected milk. Can humans also get sick from ingesting animal products that contain the virus? The FDA has found fragments of H5N1 in 20% of supermarket dairy products in 17 states.
No. For humans, flu is primarily an airborne respiratory infection. It is possible to catch it by touching your eyes or nose after touching a contaminated surface or getting a contaminated liquid—like raw milk—in your eyes, but here that’s unlikely to happen outside of a farm setting. Most milk sold in stores is pasteurized, so if you and your pet drink pasteurized milk from the supermarket, you’ll be fine.
Why haven’t more people caught it?
A lot of it comes down to biology. Birds have a type of cell receptor in their upper respiratory tract that this virus can attach to, and we don’t have that receptor.
Do we know what made the infected dairy workers susceptible to infection?
No, we don’t. It’s possible genetic vulnerabilities or compromised immune systems were at play. We also don’t know why those cases were so mild, when others have been so severe.
But a question I have is, do we really know there have been only four U.S. cases? There could be more more; if others had mild symptoms, they might not report it. We caught these cases in testing, but we’re not testing widely. We don’t even have a good grasp on how many cows are infected because there is limited testing of them as well. You’d hope after the COVID pandemic that there’d be much more surveillance and screening. Instead, we have significant gaps in information.
However, scientists are doing whatever they can. They’ve analyzed the sequence of the virus and calculated when this flu jumped from birds into cows. In the U.S., the spillover event happened around December 2023. But the current bird flu outbreak has actually been ongoing since 2021.
Since then, there have been 27 cases of human infection in eight countries, including 14 critical cases and seven deaths. What’s behind that high mortality rate?
One explanation is that the people who sickened or died were infected directly by an animal that carried the disease. Their bodies had no immunity to the virus, which explains why for humans, avian flu infections commonly cause more severe disease compared to human influenza strains. And yet despite its high pathogenicity, H5N1 has limited capacity to spread from these infected people to others. Normally influenza strains adapt as they move to different species, evolving functions that promote survival and transmissibility. Without those intermediary steps, H5N1 didn’t evolve, so it wasn’t able to spread between people.
And, as with the U.S. dairy workers, we also don’t know if individual susceptibilities contributed to the vulnerability of these infected people.
So if we start seeing evolution of the virus through intermediary species, that becomes worrisome.
Exactly. If it acquires the ability to pass from other species to humans, and then from human to human, that’s very bad news.
The major concern here is pigs. They are one of the few animals that can get infected by human, avian, and swine flus. If you have a pig infected with the human variety who then gets an avian version at the same time, the virus can recombine to create a new virus. A particularly bad combination would be a strain that combines the pathogenicity of avian flu with the transmissibility of human flu.
The swift development of COVID vaccines played a defining role in ending that pandemic. Flu vaccines already exist.
They do, and we even have avian flu vaccines available, if necessary, as well as other variants we can modify to increase our targeted vaccine stockpile. So we’re not in a situation as bad as we initially were with COVID.
You’re trying to develop a universal flu vaccine. What are the challenges?
Due to the anatomy of the virus, we’re aiming at a moving target. Like SARS-CoV-2, the surface of an influenza virion is brimming with antigens that can evolve rapidly, giving rise to new variants that we have limited immunity against. Our antibody response to influenza is typically directed at viral proteins in a region of the antigen called the head domain, which is unique to each strain. However, there is also a region called the stalk domain that is highly conserved across diverse influenza strains, which means it’s similar in each one. Unfortunately, our immune responses only rarely aim at the stalk regions, and any responses are short-lived.
So the goal is to be able to redirect our antibody responses away from the variable, strain-specific regions of the virus and get them to target these highly conserved regions, which cannot mutate very easily. If we can do that, we can target multiple variants at once, as well as provide protection against any variants that might arise in the future.
That’s the approach the Ravetch lab is taking, correct?
It’s one of them. Based on what we’ve learned about the importance of a specific set of immune pathways that are required to elicit broadly protective immunity, we are developing and testing new vaccine candidates that use these pathways to refocus the immune response towards conserved regions of the virus.
Recently, in collaboration with the Icahn School of Medicine at Mount Sinai, we examined one novel vaccine that’s in Phase 1 testing. We found that its vaccine-elicited antibodies rely on interactions with these specific immune receptors to give protection(opens in new window), which is consistent with our previous findings. Knowing this helps us get closer to designing universal flu vaccines with maximal effect.
These findings are not limited to influenza, by the way. They’re relevant for other serious viral pathogens, including SARS-CoV-2, Ebola, and HIV, as we’ve demonstrated in previous research.
How close are we to having a universal flu vaccine available?
It’s hard to estimate, but we’re definitely getting closer. Over the past several years, there has been remarkable progress. We now know more than ever before how the virus evades host immunity, what the requirements are for eliciting universal immunity against diverse influenza strains, and how our immune system responds to infection or vaccination. When you put this new knowledge together with advancing technologies and vaccine platforms, we’re really accelerating towards a universal flu vaccine. In fact, there are several candidates in clinical development and testing.
In the meantime, it’s a good idea for everyone eligible for a regular flu vaccine to get one.
Until then, do you think we’re equipped to handle whatever may come our way with avian flu?
I’m optimistic, because after COVID, we know a lot more about how to respond to pandemics. Some governments have already been considering offering avian flu vaccines to farm workers and others with high risk of exposure to avian flu. We also have an infrastructure in place that we can rely on for developing therapeutics—and one day, we’ll have better vaccines.