Schizophrenia Predisposition Linked to Two Genes on Chromosome 22
In a systematic study of 13 genes on human chromosome 22 in an area of the chromosome previously linked to schizophrenia, a team of scientists in the United States and South Africa identified two genes from this group that contribute to susceptibility to this psychiatric disorder.
The report, published in the March 12 Early Edition of Proceedings of the National Academy of Sciences, examined about half of the genes in a region of chromosome 22 called 22q11. The scientists, led by Rockefeller University researcher Maria Karayiorgou, M.D., have recently completed analysis of all the genes in this region and plan to publish a report on the remainder at a later date.
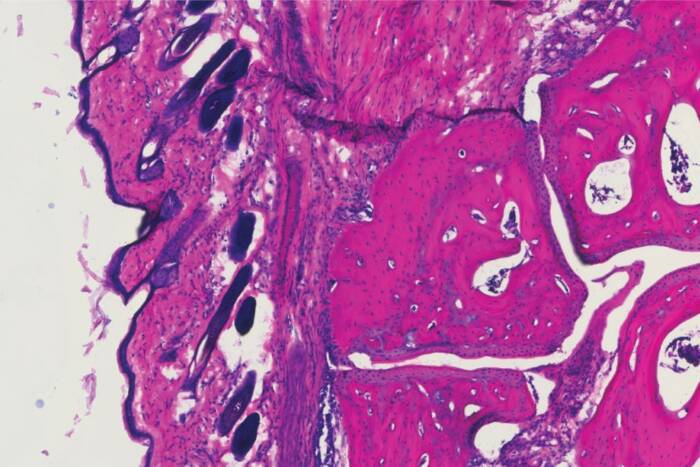
Previous studies by Karayiorgou and others revealed that 25 to 30 percent of people with microdeletions (genetic flaws that remove chunks of human chromosomes) in 22q11 develop schizophrenia, a common severe mental illness that affects 1 percent of the population and is characterized by disordered thinking as well as deficits in emotional and social behavior.
The role of 22q11 microdeletions in schizophrenia were strengthened by additional studies by Karayiorgou and others showing that these microdeletions occur in up to 2 percent of adult schizophrenic patients and up to 6 percent of patients with childhood onset schizophrenia, a particularly aggressive form of the disease that causes symptoms in children by age 13.
In the general population, about 1 in 4000 people (0.025 percent) have 22q11 microdeletions.
The scientists hypothesized that while deletions of genes from chromosome 22q11 may account for only a small proportion of schizophrenia cases in the general population, other types of more subtle genetic flaws such as common variants of individual genes from the 22q11 region may make a larger contribution in non-deleted schizophrenic patients in the wider population.
In the research reported in PNAS, scientists examined 22q11 in 242 non-deleted people affected by schizophrenia and their parents, as well as people not diagnosed with schizophrenia, focusing on variations in 13 genes in that region.
The 242 affected individuals were taken from three independent patient populations: 107 adult schizophrenics from North America, 26 children diagnosed with childhood onset schizophrenia and 109 schizophrenic patients of South African Afrikaner origin.
The researchers found variants in two genes, PRODH2 and DGCR6, enriched in patients with schizophrenia as compared to unaffected individuals who served as “normal controls” for the study. Two additional lines of evidence showed that of the two genes, PRODH2 may play a more important role.
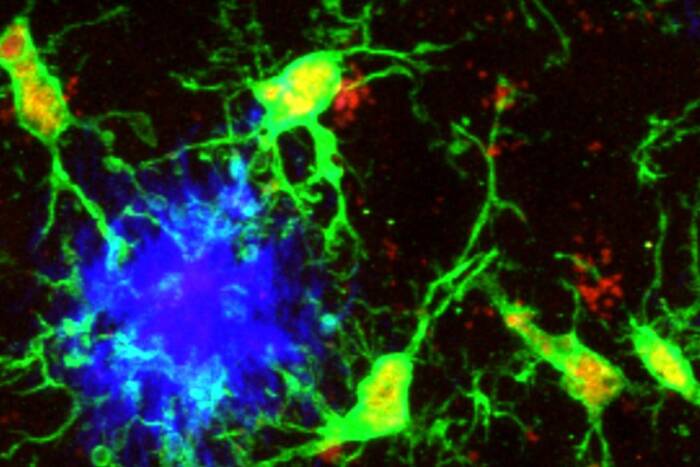
First, experiments on a PRODH2-deficient mouse conducted by Karayiorgou’s lab in 1999 revealed deficits in sensorimotor gating, which is the ability to filter sensory inputs such as sounds. Sensorimotor gating is also affected in people with schizophrenia.
Second, Karayiorgou and her colleagues, by analyzing the publicly available sequence of chromosome 22, discovered a linked “pseudogene” of PRODH2. The pseudogene, which is 97 percent similar to the true gene in its DNA sequence, does not produce a functional protein.
The researchers discovered that the PRODH2 pseudogene serves to introduce missense mutations—mutations leading to amino acid substitutions that produce a nonfunctioning protein—in the gene that confer susceptibility through a process called gene conversion.
“Pseudogene-like variations of PRODH2 may prevent synthesis of a fully functional enzyme and seem important for increasing susceptibility to schizophrenia because they are present either exclusively or in higher frequencies in people with schizophrenia as compared to controls,” says Karayiorgou, associate professor and head of the Laboratory of Human Neurogenetics at Rockefeller. “We also suspect that these variations modulate the onset age of schizophrenia.”
The sequencing of the human genome has revealed thousands of pseudogenes. An implication of this work is that it points to pseudogenes as a possible constant and renewable source of variation that can be effectively transferred to linked susceptibility genes via gene conversion.
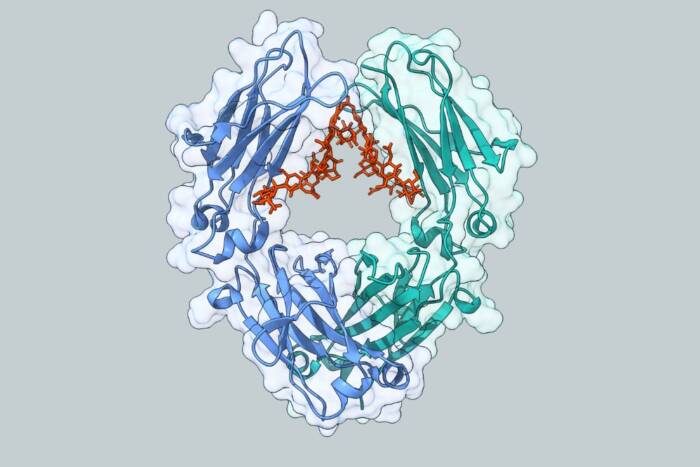
PRODH2 encodes for a brain enzyme called proline dehydrogenase, which is involved in neuron signal transmission as well as cell death.
“The particular pathway in which PRODH2 is involved is largely undescribed, and is a novel pathway that will open up several different avenues for new drug development,” she says.
Karayiorgou’s co-authors are Hui Liu, Christina Sobin, Brandi L. Galke and Maude L. Blundell at Rockefeller; Simon C. Heath at Memorial Sloan-Kettering Cancer Center; J. Louw Roos at the University of Pretoria, Republic of South Africa; Marge Lenane and Judith L. Rapoport at the National Institute of Mental Health; Brian Robertson at the University of Capetown, Republic of South Africa; Ellen M. Wijsman at the University of Washington; and Joseph A. Gogos at Columbia University College of Physicians and Surgeons.
This work was supported by grants from the New York Academy of Medicine, the EJLB Foundation, the Essel Foundation and the Norman and Rosita Winston Foundation. Clinical work at The Rockefeller University Hospital General Clinical Research Center was supported in part by a grant from the National Institutes of Health